History
Diagnosis
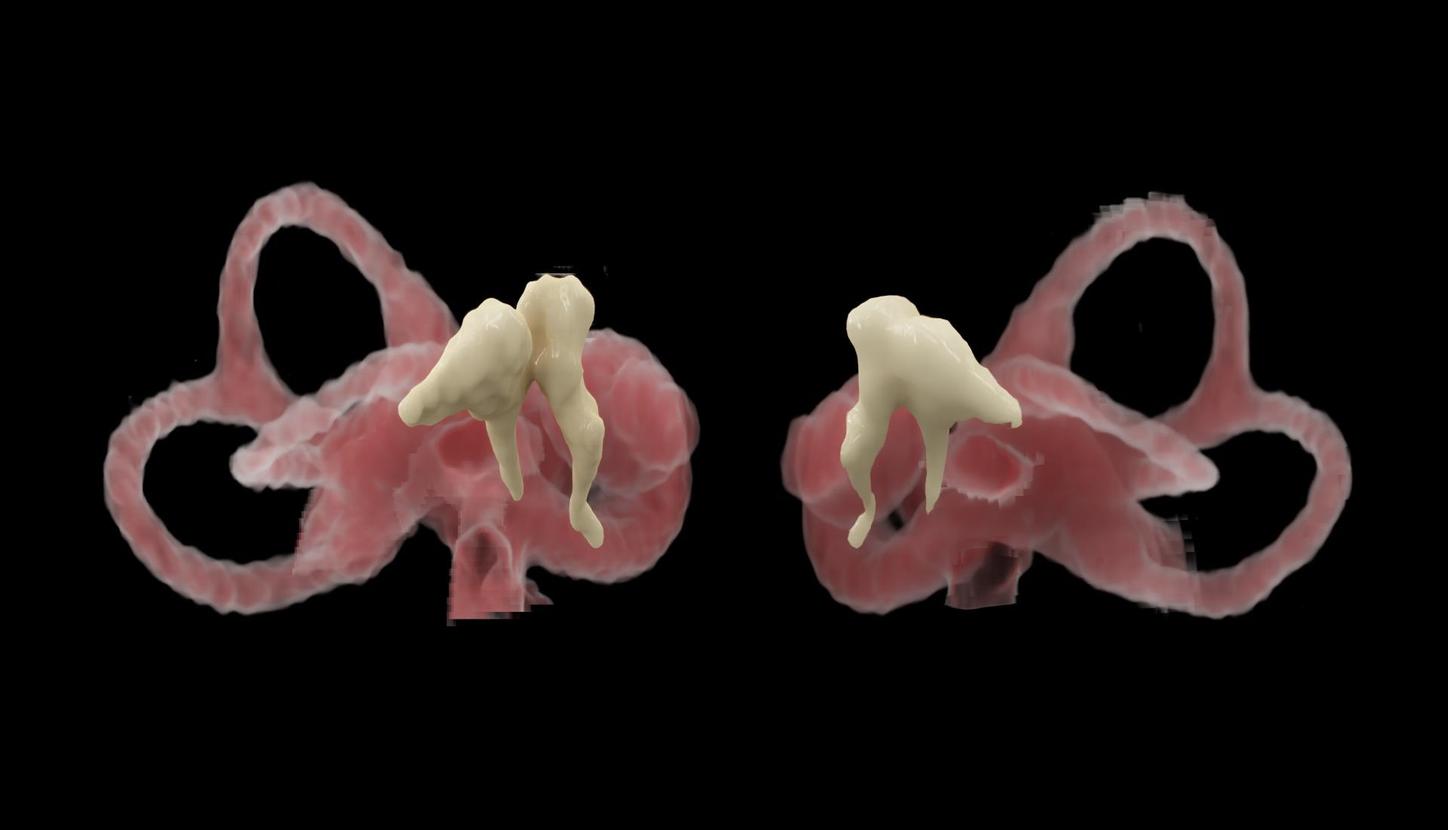
CT images showed an incudomalleolar dislocation with a typical “broken heart” sign in the thin-slice coronal multiplanar reformats (MPR). The displacement of the head of the malleus from the body and short process of the incus disarticulating the normal “ice cream cone” of the joint was also seen in axial images (Fig. 1). These structures were visualized in more details in zoomed reconstructions (Fig. 2). Longitudinal fractures of the right temporal bone (Fig.3a), involving the mastoid cells, the external auditory canal, the middle ear and the ossicles, as well as a complex fracture of the body of the sphenoid bone were present (Fig.3b and 3c). Temporal subdural hematoma, subarachnoid bleeding as well as parenchymal brain contusion injuries on the left, due to the contrecoup mechanism, were seen. There was no evidence of extracranial traumatic lesions. A subsequent control CT examination demonstrated stable contusional injuries with mild progression of the perifocal edema and a regressing subdural hematoma. Immediate neurosurgical intervention was not considered. The patient was treated conservatively on the intensive care unit for two days and was then transferred to the traumatology ward. Ear-nose-throat (ENT) consultation found a right-sided conductive hearing loss.
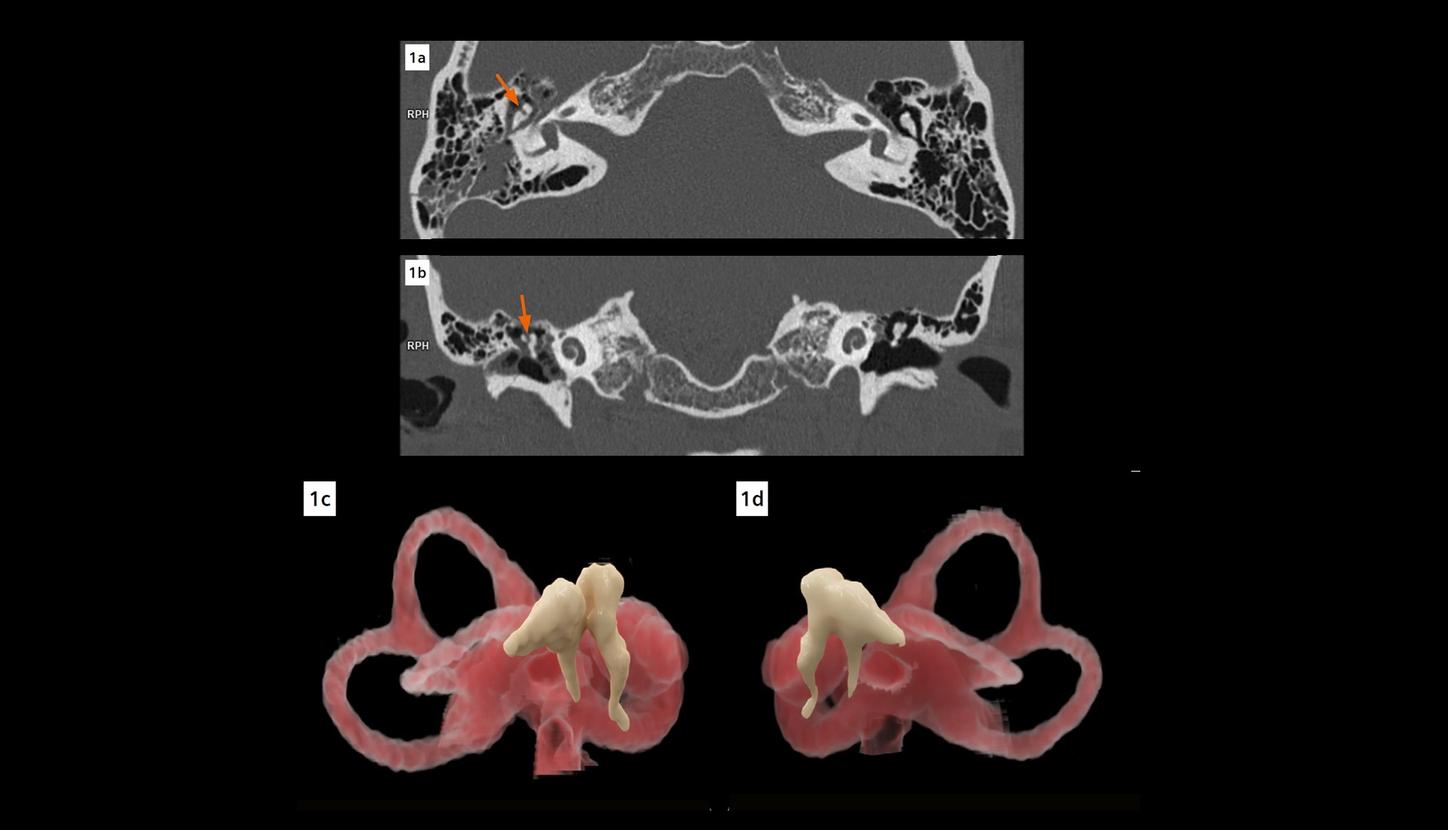
Fig. 1: An axial image (Fig. 1a) shows displacement of the head of the malleus from the body and short process of the incus (arrow) on the right. A typical “broken heart” sign (arrow) is seen in a coronal MPR image (Fig. 1b). Two cVRT images (Figs. 1c and 1d) created with thin slices (0.4 mm, sharp kernel of Hr76) demonstrate the incudomalleolar dislocation (Fig. 1c) in three dimensions.
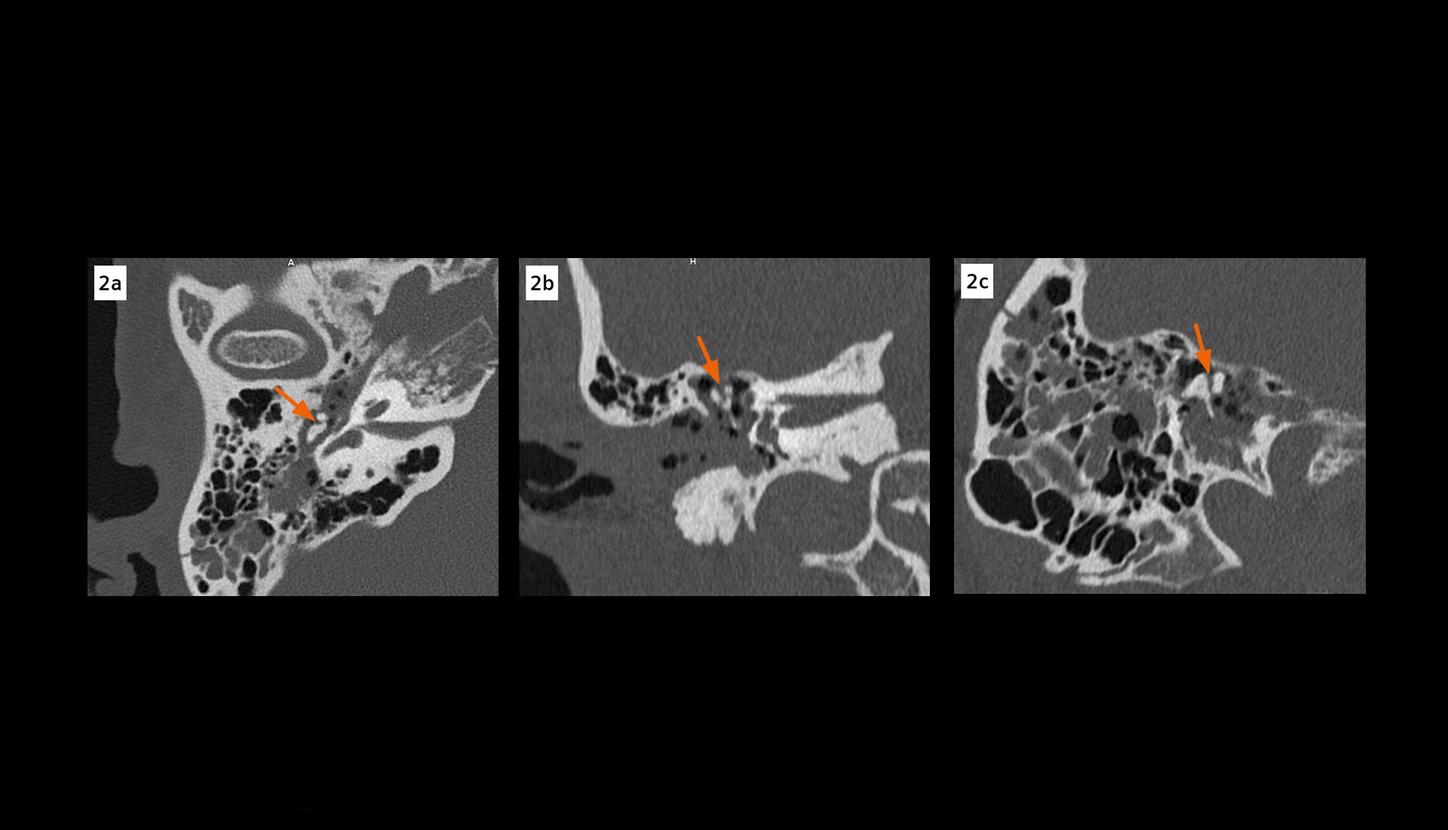
Fig. 2: Images from zoomed reconstructions show the incudomalleolar dislocation (arrows) with signs of disarticulated “ice cream cone” (Fig. 2a) and “broken heart” (Fig. 2b) in details.
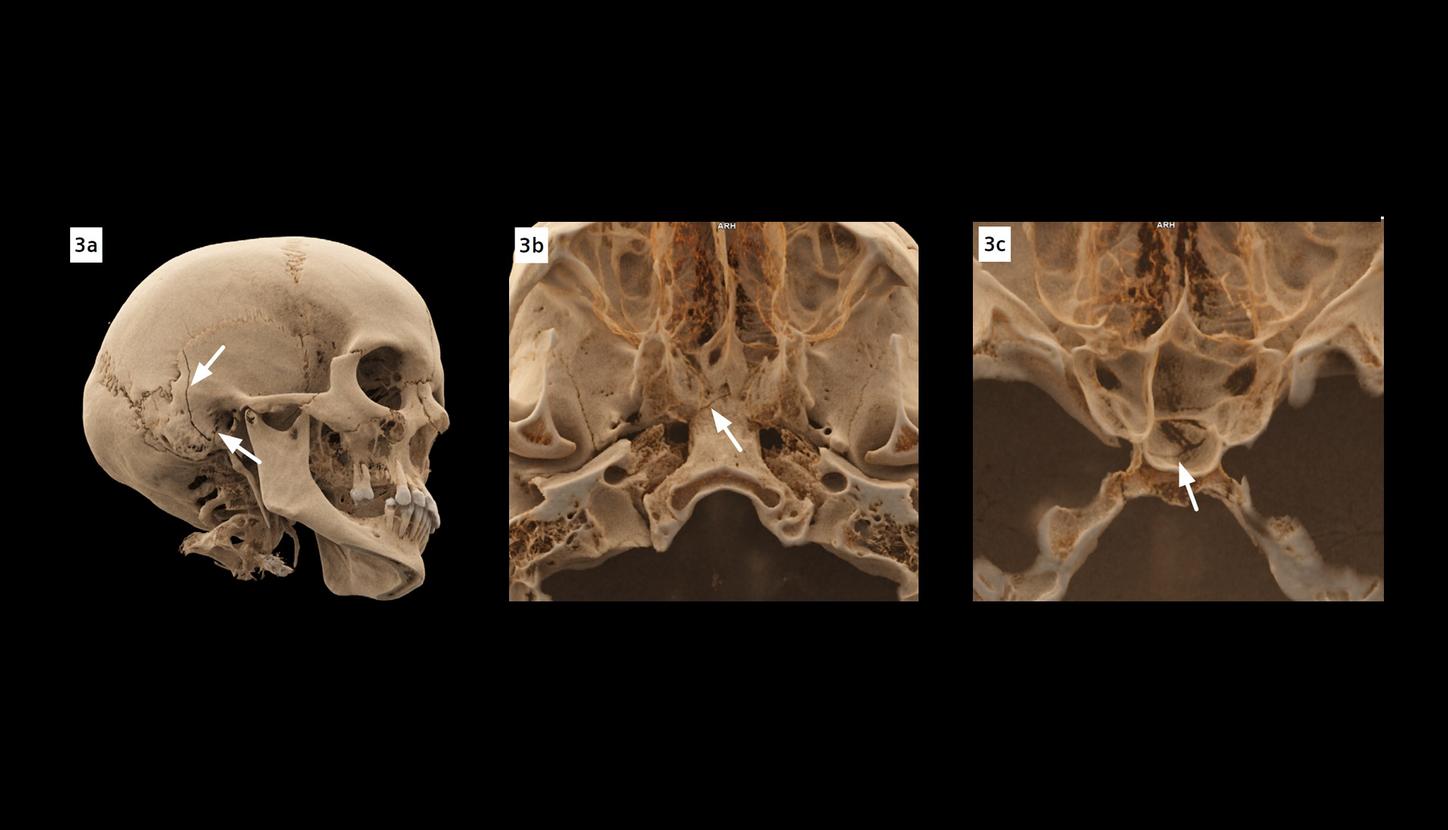
Fig. 3: cVRT images show longitudinal fractures (Fig. 3a, arrows) of the right temporal bone, involving the mastoid cells and the external auditory canal, as well as a complex fracture of the body of the sphenoid bone (Fig. 3b and 3c, arrows).
Comments
Examination Protocol