History
A 47-year-old male patient, complaining of persistent upper abdominal pain for the past month, presented himself to the hospital for a check-up. An initial contrast-enhanced CT examination was performed on a conventional energy-integrating detector (EID) CT. This revealed an ill-defined hypo-enhancing mass in the pancreatic body, accompanied by distal pancreatic atrophy, dilation of the main pancreatic duct, splenic vein occlusion and collateral vessel formation. Two critical diagnostic concerns emerged: (1) heterogeneous attenuation within the adjacent main pancreatic duct raising suspicion of an intraductal tumor spread; (2) a ~5 mm hypoattenuating lesion in the hepatic segment IV, exhibiting indistinct margins and equivocal enhancement, raised concerns about a potential metastasis. With informed consent, another contrast-enhanced CT scan was performed three weeks later using an ultra-high resolution (UHR) mode with a photon-counting detector (PCD) CT, NAEOTOM Alpha, for further evaluation.
Diagnosis
Virtual monoenergetic images (VMI), displayed at 50 keV, revealed a distinctly delineated tumor with clear margins (39 × 24 mm in axial plane; 24 mm height in coronal view) in the pancreatic body, causing notably encasement of the splenic artery and occlusion of the splenic vein. Thickening and enhancement of the left celiac ganglion, not shown in previous EID CT, were seen as suspicious of a metastasis. Both prior imaging ambiguities were clearly resolved – the fluid attenuation within the main pancreatic duct was homogeneous, therefore ruling out intraductal tumor spread, and the hepatic lesion in segment IV was non-enhancing with a sharp delineation characterizing a cyst. A pancreatic ductal adenocarcinoma with perineural invasion (metastasis of the left celiac ganglion) was suggested and subsequently confirmed by pathological analysis after a successful radical distal pancreatectomy with splenectomy and a partial portal vein reconstruction. The patient recovered uneventfully.
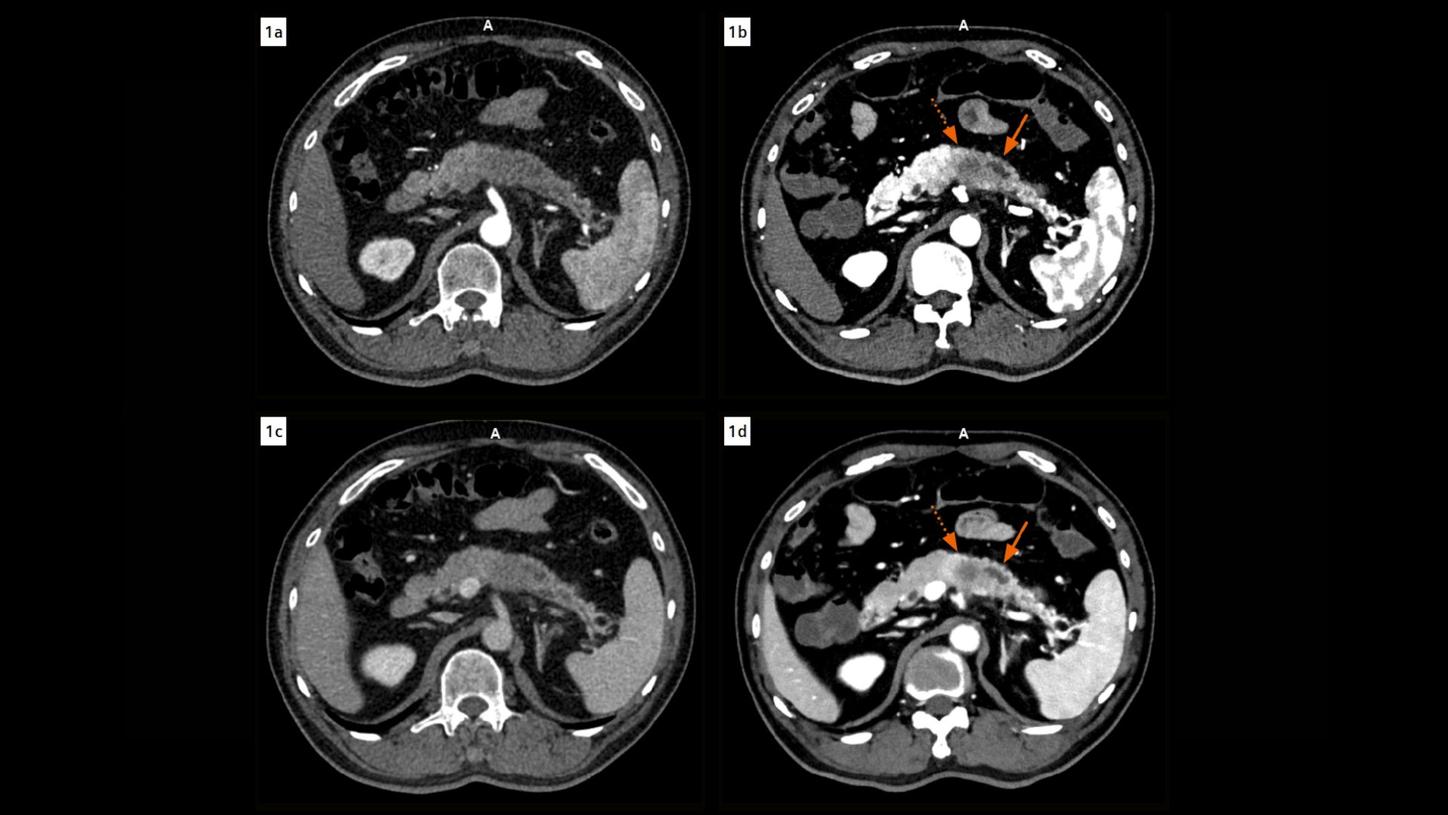
Fig. 1:ĚýAxial images acquired during the arterial (Figs. 1a & 1b, EID at 1 mm, PCD at 0.4 mm) and venous phases (Figs. 1c & 1d, 3 mm) show a comparison of CT findings in the pancreas in EID (Figs. 1a & 1c) and PCD CT images (Figs. 1b & 1d). The fluid attenuation within the main pancreatic duct (arrows) adjacent to the tumor appears heterogeneous in EID CT images, however, clearly homogeneous in PCD CT images, ruling out the suspicion of an intraductal tumor spread. The tumor is distinctly delineated with clear margins in the PCD CT images (dotted arrows). Note the improved contrast in PCD CT images using VMIs displayed at 50 keV.Ěý
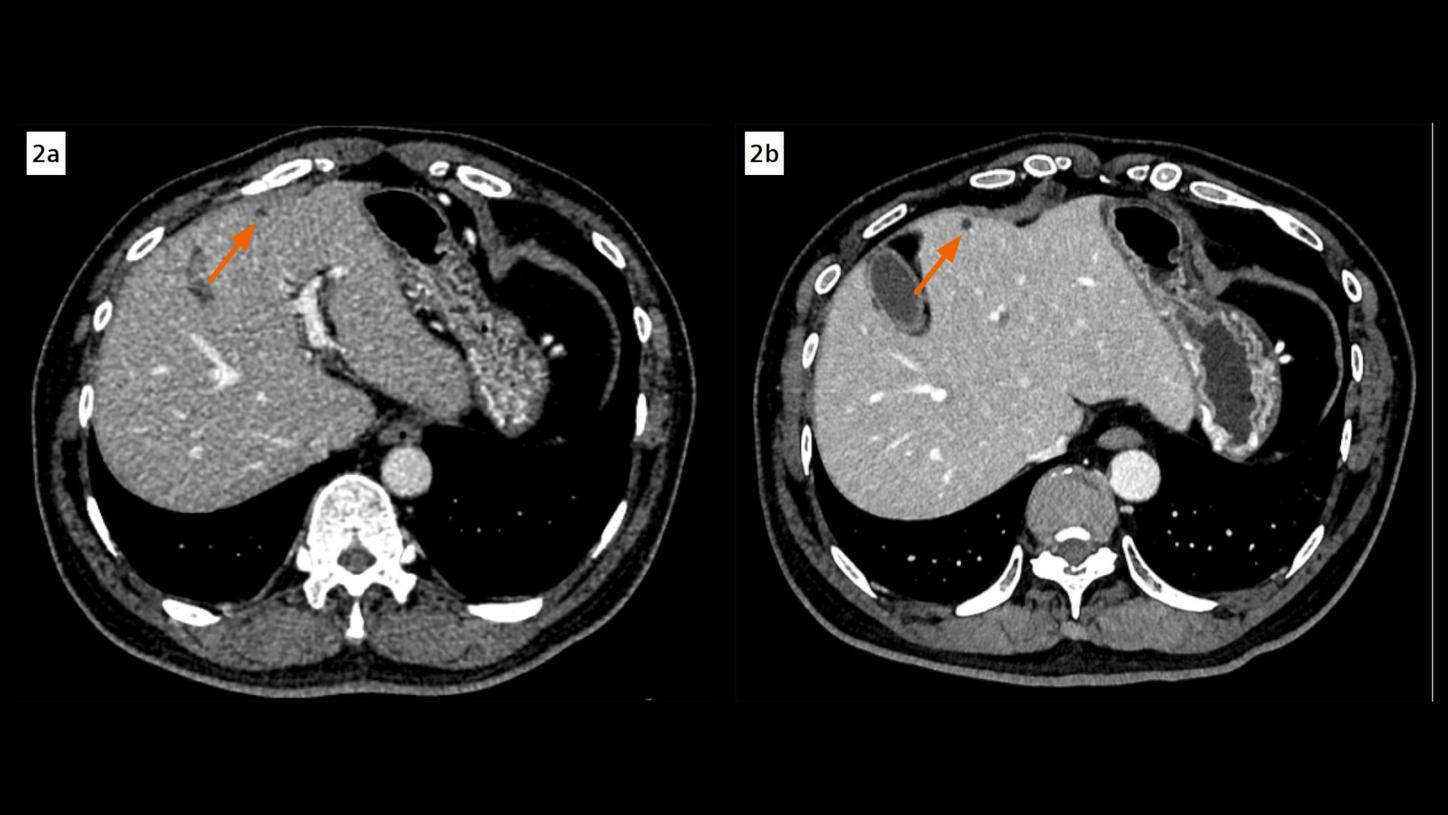
Fig. 2:ĚýA hypoattenuating lesion in the hepatic segment IV, exhibiting indistinct margins and equivocal enhancement in an EID CT image (Fig. 2a, arrow), is clearly characterized as a non-enhancing, sharply delineated cyst in a PCD CT image (Fig. 2b, arrow). Both images are reconstructed at 1 mm, displayed at same window settings. The image noise is notably less in the PCD CT image.
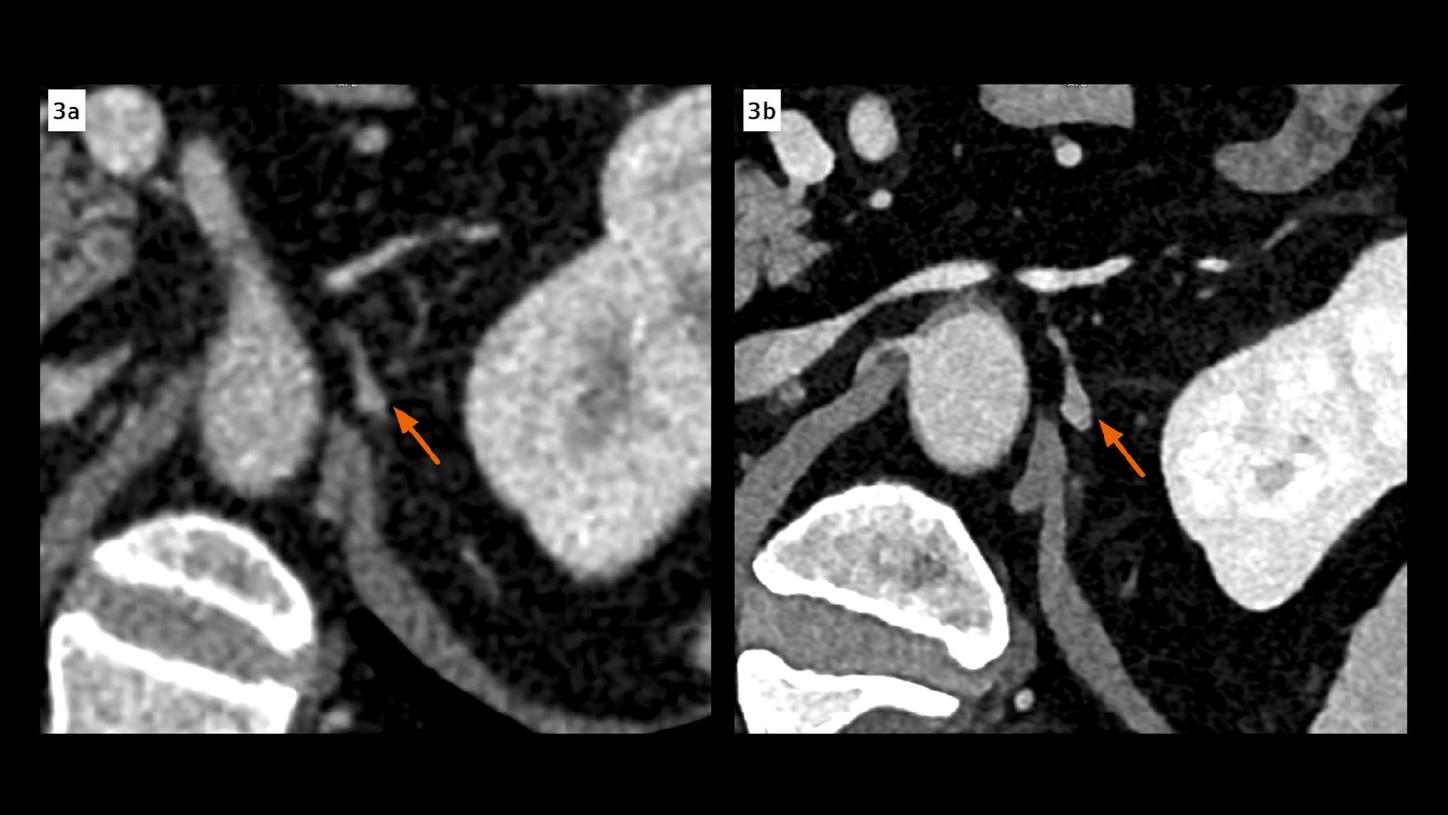
Fig. 3:ĚýThickening and enhancement of the left celiac ganglion, not shown in an EID CT image (Fig. 3a, arrow, 1 mm), is clearly seen in a PCD CT image (Fig. 3b, arrow, 0.4 mm), indicating a metastasis. It is also confirmed by pathological analysis after surgery. Both images are displayed at same window settings. Note the improved contrast in the PCD CT image using a VMI displayed at 50 keV.Ěý
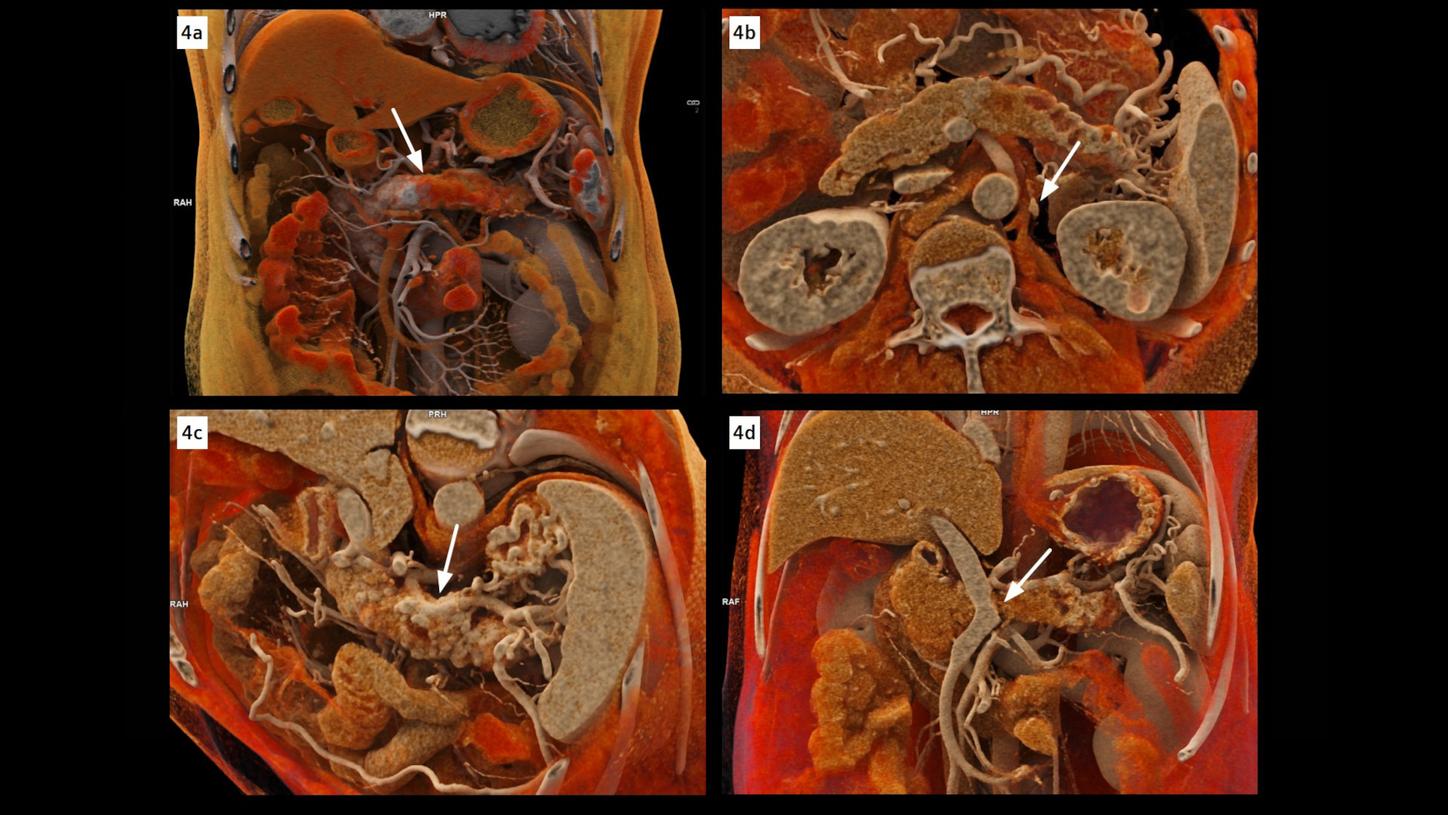
Fig. 4:ĚýcVRT images show a distinctly delineated tumor in the pancreatic body (Fig. 4a, arrow), causing notably encasement of the splenic artery (Fig. 4c, arrow), and occlusion of the splenic vein (Fig. 4d, arrow). The left celiac ganglion (Fig. 4b, arrow), thickened and enhanced, is confirmed as a metastasis by pathological analysis after surgery. Images reconstructed at 0.2 mm with a sharp kernel of Bv48 are used to create these cVRT images.
Comments
Accurate preoperative imaging is crucial in pancreatic cancer, yet conventional EID CT often struggles to delineate tumor boundaries and assess adjacent structures – particularly in hypo- or isoattenuating lesions – leading to potential misjudgments in resectability. [1]
PCD CT offers significant technical advances, including improved spatial resolution, reduced image noise and intrinsic spectral imaging. [2,3] These features enhance tumor conspicuity and allow improved visualization of both vascular and neural invasion. Emerging evidence has suggested that PCD CT outperforms conventional EID CT in abdominal imaging, supporting its growing value in preoperative assessment and surgical planning. [4,5].
In this case, these advantages translated into clear clinical impact – PCD CT not only improved tumor conspicuity and delineation of peripancreatic neural invasion, but also confidently resolved two critical diagnostic ambiguities: the suspected intraductal tumor spread and the potential hepatic metastasis, either of which could have altered surgical management.
These benefits were achieved through the use of an UHR scan mode, in which small sub-pixels are defined by electric fields rather than physical separations and are read out separately to increase the spatial resolution with improved geometrical dose efficiency of the detector. Simultaneously, spectral information was acquired, allowing for increased image contrast by displaying VMI at low keV (50 keV in this case). This unique combination provides improved image sharpness and contrast-to-noise ratio, helping the characterization of small lesions and anatomical details, especially in soft tissue. These UHR images are also optimized for in-depth three-dimensional image rendering, using cinematic volume rendering technique (cVRT), facilitating communication with the clinicians. It is also worth noting that a Flash mode (pitch of 2.35) with a collimation of 96 x 0.2 mm is performed to achieve a fast acquisition of the arterial phase (2.8 s), using the advantage of dual source CT scanning, further improving the visualization of vascular details.
This case highlights how the combination of ultra-high spatial resolution with low-keV spectral imaging can translate into actionable diagnostic confidence, enabling not only accurate local staging in pancreatic cancer but also better-informed surgical strategies through enhanced visualization of critical anatomical details.
Examination Protocol

