Prostate cancer treatment demands precision to balance effective therapy with minimal side effects. Advances in the use of MRI for simulation and planning in radiation therapy have revolutionized how clinicians visualize and target tumors, offering new possibilities for tailored and adaptive care. These innovations are reshaping the landscape of prostate cancer management.
MRI has transformed prostate cancer treatment, offering precision in identifying key anatomical and tumor-related features. MRI reliably delineates the prostate, areas of high tumor burden, erectile tissues, and the prostatic apex—a region with a high tumor incidence that is critical for treatment planning.1,2 By enabling more accurate identification of smaller tumor volumes, MRI reduces the risk of overestimating target areas, sparing nearby organs at risk (OARs) and enhancing the therapeutic ratio.3 Additionally, MRI helps optimize dosimetry, minimize unnecessary irradiation of seminal vesicles, and reduce toxicity during treatment.4
MRI’s role in accurate prostate tumor delineation and treatment optimization
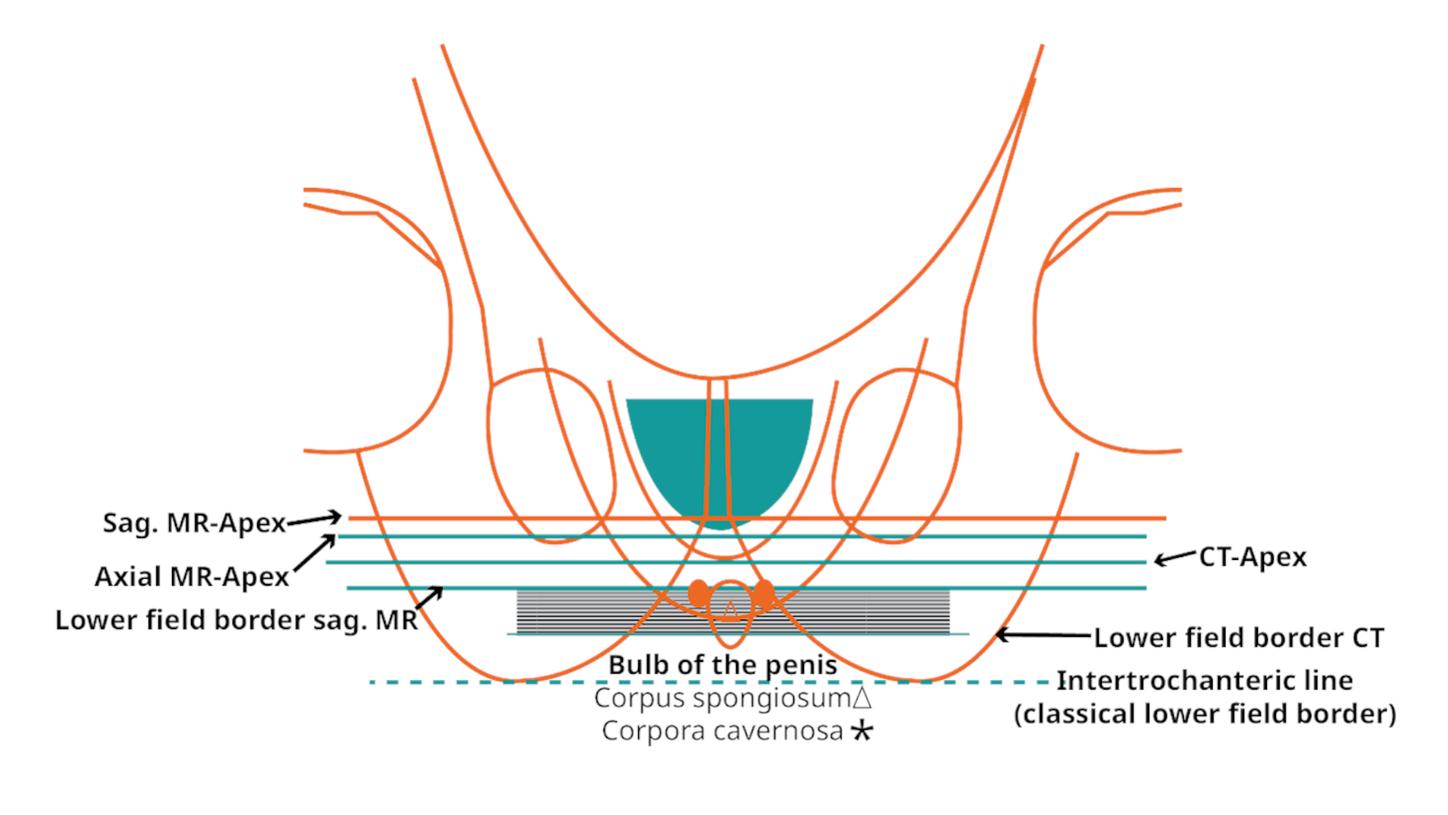
MRI’s visualization over CT in prostate tumor delineation is well documented. A study of 22 patients demonstrated that MRI significantly outperformed CT in identifying the prostatic apex, with reduced interobserver variability (P<0.001 and P=0.009, respectively). The authors concluded that MRI should be recommended for every patient’s treatment planning.5
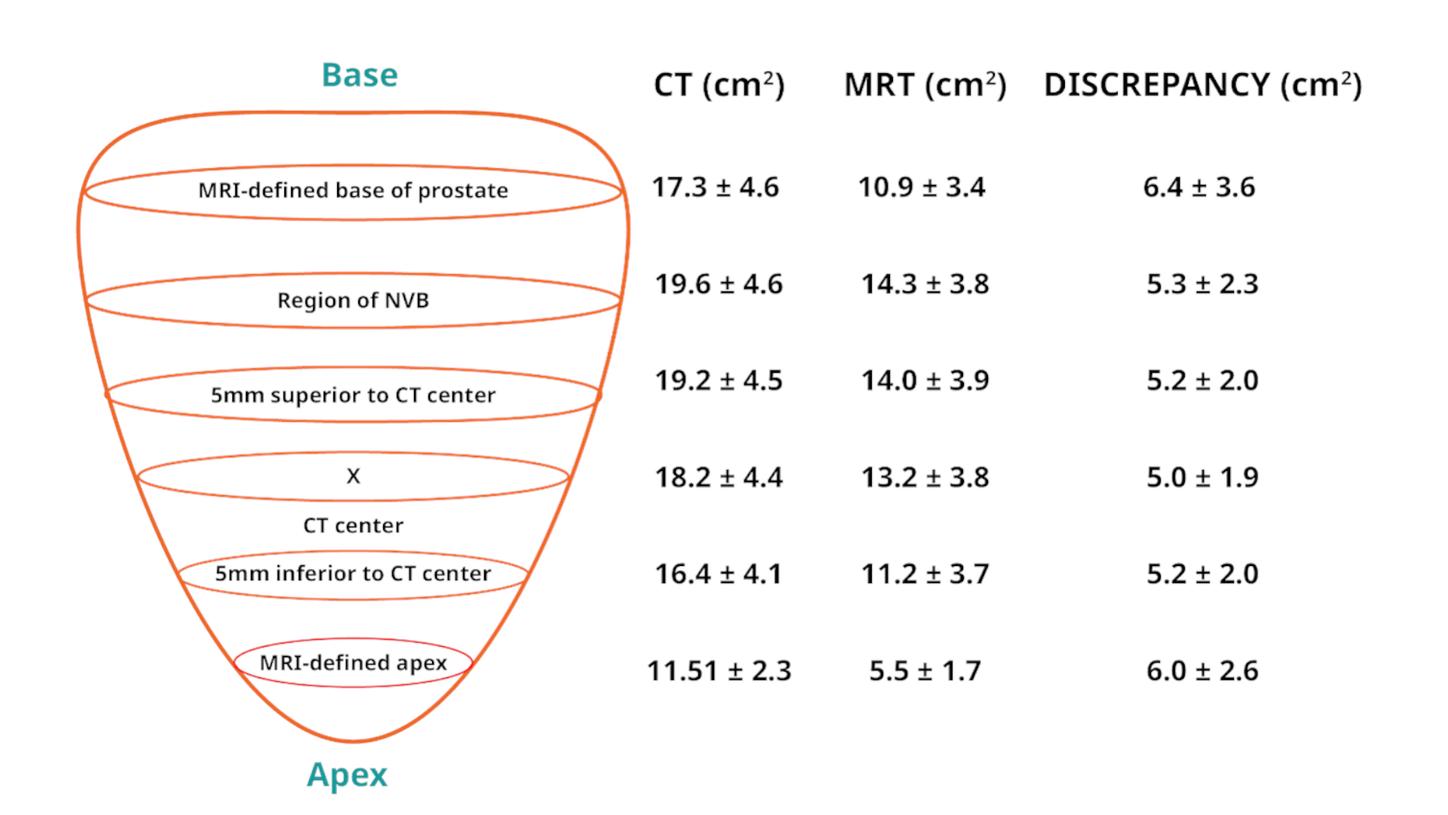
Similarly, a study of 294 patients found that prostate volumes delineated by MRI were, on average, 35% smaller than those identified by CT (P<0.001). This reduction in overestimation minimizes unnecessary exposure to OARs and enhances treatment precision.3 MRI also identifies subgroups of patients for whom seminal vesicle irradiation can be avoided, further optimizing care.3ĚýMRI-based tumor delineation improves dosimetry, allowing for safer dose escalation. In a study by Steenbakkers and colleagues, MRI-based planning enabled a dose increase of 2.0 to 7.0 Gy while maintaining the same rectal wall dose, underscoring its ability to achieve superior precision and healthy tissue sparing.4
The benefits of MRI-based adaptive planning in prostate cancer
Offline adaptive planning, particularly with MRI, complements and enhances CT-based radiotherapy workflows by addressing challenges in anatomical visualization and target definition. While CT remains the backbone of simulation and dose calculation due to its geometric accuracy and electron density information, its limitations in soft tissue contrast can introduce variability in gross tumor volume (GTV) delineation, especially in anatomically complex or low-contrast regions.6-8
MRI’s superior soft tissue contrast augments CT-based planning by refining target delineation, reducing overestimation of volumes, and minimizing radiation exposure to surrounding healthy tissues.9 This is particularly important in the context of steep dose gradients designed to spare organs at risk (OARs), where anatomical precision is paramount.
In addition, MRI’s lack of ionizing radiation makes it well-suited for serial imaging, enabling clinicians to monitor treatment response and account for tissue changes throughout the course of therapy.10 When used for offline adaptive planning, MRI-to-MRI registration provides a consistent and reliable basis for re-planning, mitigating variability introduced by inter-modality registration and setup differences.9
By integrating MRI’s strengths into the CT-based radiotherapy paradigm, offline MRI-based adaptive planning offers a more complete and responsive approach, supporting improved anatomical accuracy, treatment precision, and outcomes, particularly in prostate cancer care.10
Diffusion-weighted imaging in prostate cancer
The integration of MRI with diffusion-weighted imaging (DWI) strengthens the diagnostic and treatment capabilities for prostate cancer, offering significant benefits in terms of sensitivity and accuracy. A study found that apparent diffusion coefficient maps from DWI at a b value of 1,000 s/mm²— which measures the strength of diffusion weighting in an image—had higher sensitivity (88%) and accuracy (89%) than those at higher b values. The finding shows MRI to be a more effective tool for distinguishing cancerous from benign tissues.11 This high level of precision in tumor localization and characterization aids in accurate staging and planning so that biopsies and treatment strategies can be tailored to the individual patient. By refining tumor localization and staging, MRI with DWI not only guides precise biopsies and treatment decisions but also sets the foundation for more accurate simulation and planning in radiation therapy.