History
A 47-year-old female patient, complaining of effort dyspnea, came to the hospital for a check-up. Physical examination revealed an ejection murmur at the apical and left parasternal region. An ECG at rest showed marked ST depression and negative T waves (strain type) in leads I, aVL, V5 and V6. An ergometry test was performed, however it had to be terminated, due to significant horizontal ST depression in multiple leads. A performed echocardiography showed a slightly dilated left ventricle with a mid-range ejection fraction (EF, 44%) and systolic function. A cardiac CT angiography (CCTA) was performed on a photon-counting CT, NAEOTOM Alpha, to assess the coronary arteries.
Diagnosis
CCTA images showed an anomalous origin of the left main coronary artery (LM), arising posteriorly from the main pulmonary artery (MPA) above the pulmonary valve. The LM was ectatic, branching into the left anterior descending (LAD) artery and the circumflex (Cx). Both of which were also dilated. A connection between the proximal Cx and the MPA was seen. The right coronary artery (RCA), dilated and tortuous, was dominant with a normal origin. An enlarged descending septal artery (DSA), branching out of proximal RCA, was visualized. The LAD and the posterior descending artery (PDA) were distally connected. Collateral formation between the posterior lateral branch (PLB) and the Cx was evident. The left ventricle (LV) was slightly dilated. There were no extracardiac findings as well as no signs of coronary atherosclerosis or lumen narrowing. A Bland-White- Garland syndrome was diagnosed.
Subsequently, the patient underwent surgical repair at an external institution, where the cardiac surgery team performed a LM reconstruction and closed the connections both between the LM and the MPA, and the proximal Cx and the MPA. Postoperative imaging on an energy-integrating detector (EID) CT scanner confirmed a healthy coronary ostium without severe stenosis. The patient was sent to rehabilitation therapy and has now fully recovered.

Fig. 1: A cVRT image (Fig. 1a) and an oblique MPR image (Fig. 1b) show an anomalous origin of the LCA, arising posteriorly from the MPA (arrows). A connection between the proximal Cx and the MPA (Fig. 1a, dotted arrow) is also seen. The LV is slightly dilated.

Fig. 2: cVRT images show a dilated and tortuous RCA and its branches. The LAD and the PDA are distally connected (Fig. 2a, arrow). A collateral between the PLB and the Cx (Fig. 2b, arrow) is also seen.
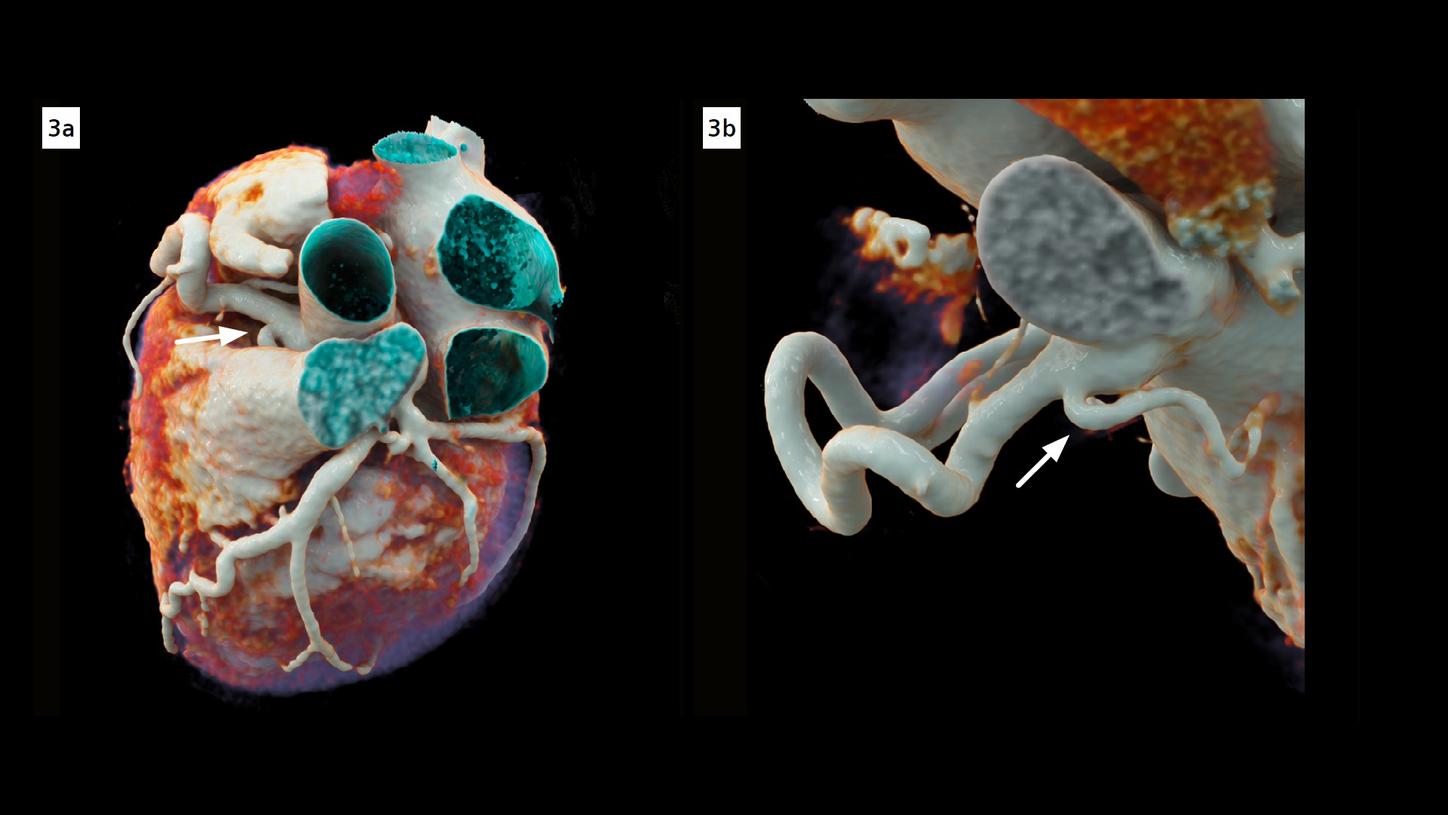
Fig. 3: cVRT images show an enlarged DSA branching out of the proximal RCA (arrows). Both left and right coronary arteries are dilated and tortuous.

Fig. 4: cVRT images show a reconstructed LM (arrows) with a healthy ostium without severe stenosis.
Comments
Bland-White-Garland syndrome, also known as anomalous left coronary artery arising from the pulmonary artery (ALCAPA), is one of the most serious congenital coronary artery anomalies. If left untreated, approximately 90% of infants die within their first life year. Manifestation in adults occurs only in rare cases, presenting symptoms of chronic myocardial ischemia, arrhythmias, heart failures or even sudden cardiac arrest. Curative treatment is surgical repair. CT imaging is noninvasive, allowing for direct visualization of the anomalous origin, course of the coronary arteries and collateral formation, providing important information for treatment planning.
This case was performed on a dual source, photon-counting detector (PCD) CT, NAEOTOM Alpha. It provides a combination of high spatial and temporal resolution, enabling the acquisition of small details, such as collateral formation. Spectral information, available in routine scans, allows image display at low keV (55 keV in this case) enhancing image contrast. The optimal image quality achieved can also be demonstrated in three dimensions, with improved depth and shape perceptions, using cinematic volume rendering technique (cVRT). This facilitates the communication with the surgeons, and subsequent surgical planning.
Examination Protocol
