Impressive clinical outcomes
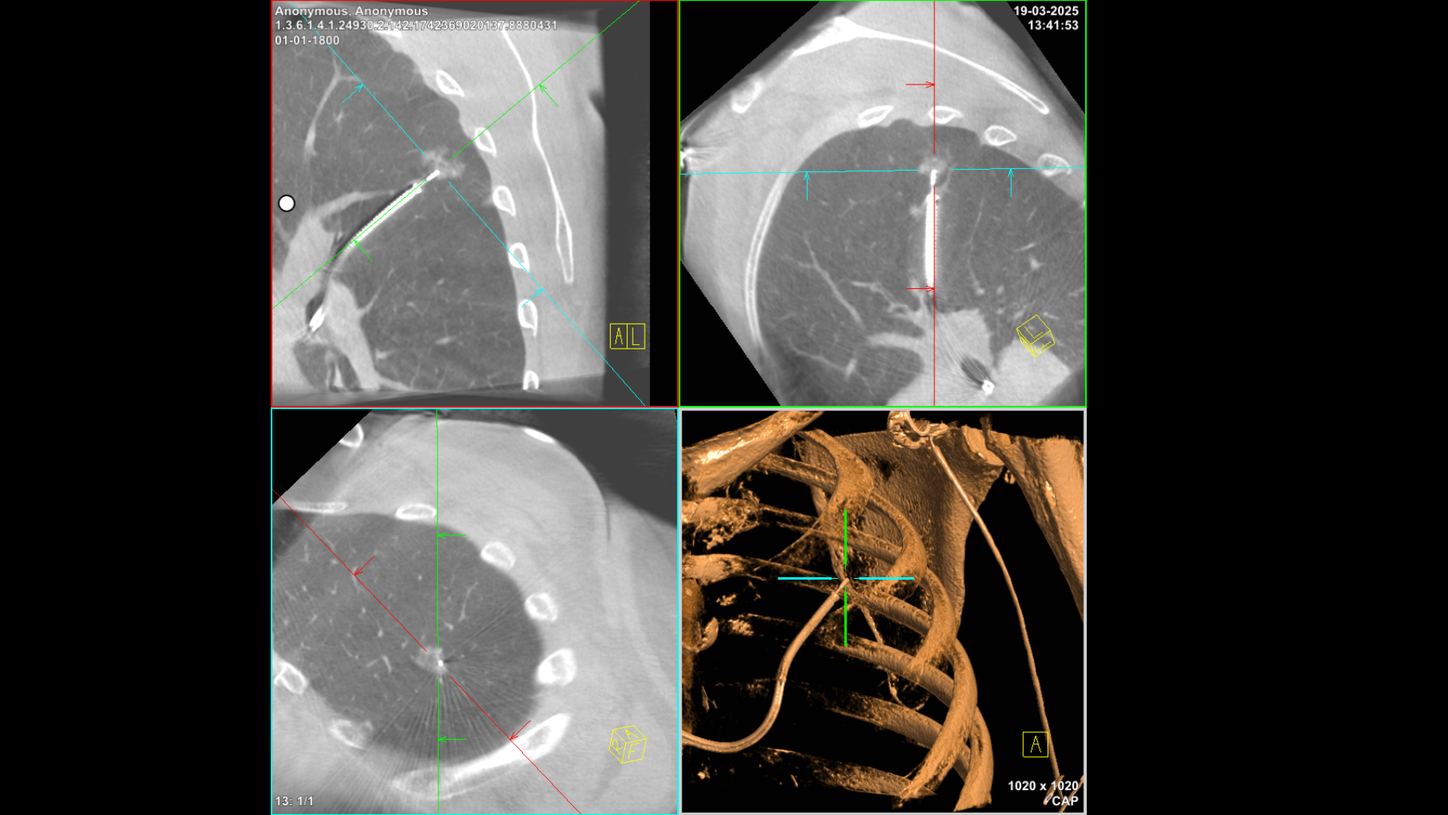
The solution’s precision has yielded remarkable results, with a 99 percent tool-in-lesion rate and an 89.3 percent diagnostic yield2 (strict definition, 10 mm median lesion size, 15% positive bronchus sign). “For about 90 percent of all the patients undergoing robotic-assisted bronchoscopy with integrated cone beam CT, we were able to get a diagnosis,” says Gaisl. “We successfully accessed a new patient group without negatively impacting our existing manual bronchoscopy program.”
Combining cone beam CT with robotic-assisted bronchoscopy has several additional advantages, as Gaisl explains: “First, complexity goes down for everyone. This means we can do more procedures a day. The procedure time for robotic-assisted bronchoscopy with cone beam CT is 37 minutes. This is similar to the 34 minutes needed for conventional bronchoscopy with 2D fluoroscopy [2]. Second, the radiation dose for each patient goes down. Third, we’re also able to see where we are in the lesion. Sometimes the integration is so helpful that we no longer need a second 3D spin. At USZ, the average is 1.25 spins per lesion [2].”

Comprehensive nodule management
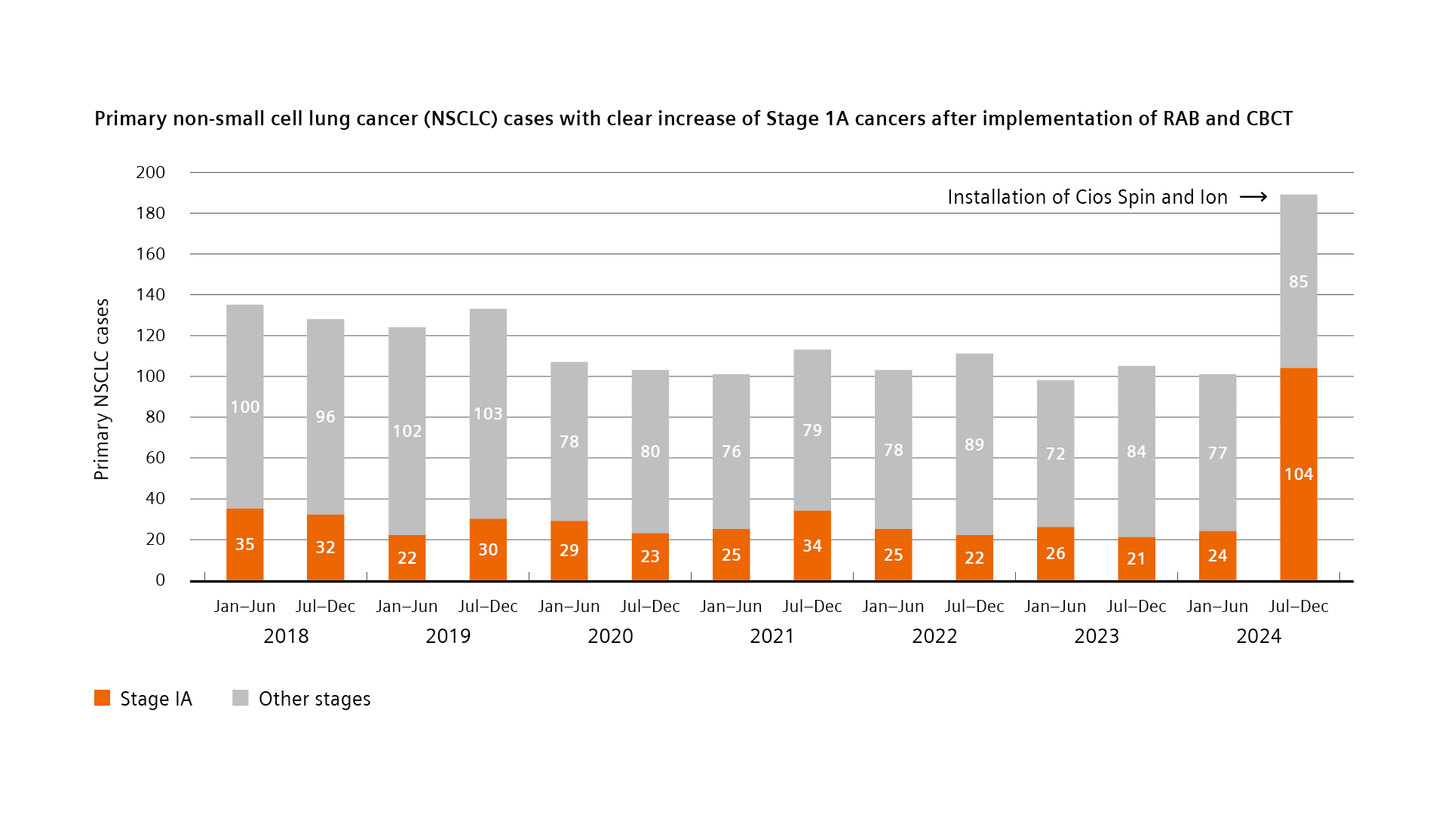
Success with this technology requires a systematic approach. “In order to achieve a stage shift for lung cancer diagnosis, we introduced the lung nodule board at our institution,” explains Gaisl. “The members of the board are dedicated thoracic radiologists, thoracic surgeons, and pulmonologists, who can then make sure that all the resources we have available are adequately allocated, and that the right patients get the right biopsy and treatment at the right time.” In addition to the much better survival outcomes, earlier detection also has substantial economic implications. According to current data, monthly excess expenditures for lung cancer treatment increase significantly with disease progression, ranging from approximately €3,228 for Stage IA cancer to €8,293 for Stage IVB cancer3.

Future impact on global health
With lung cancer remaining the leading cause of cancer-related mortality worldwide, accounting for over 1.8 million deaths annually according to WHO data1, this technological advancement represents a significant step forward. The ability to detect and diagnose lung cancer at earlier stages through robotic-assisted bronchoscopy with integrated cone beam CT could fundamentally alter the trajectory of patient outcomes in thoracic oncology.