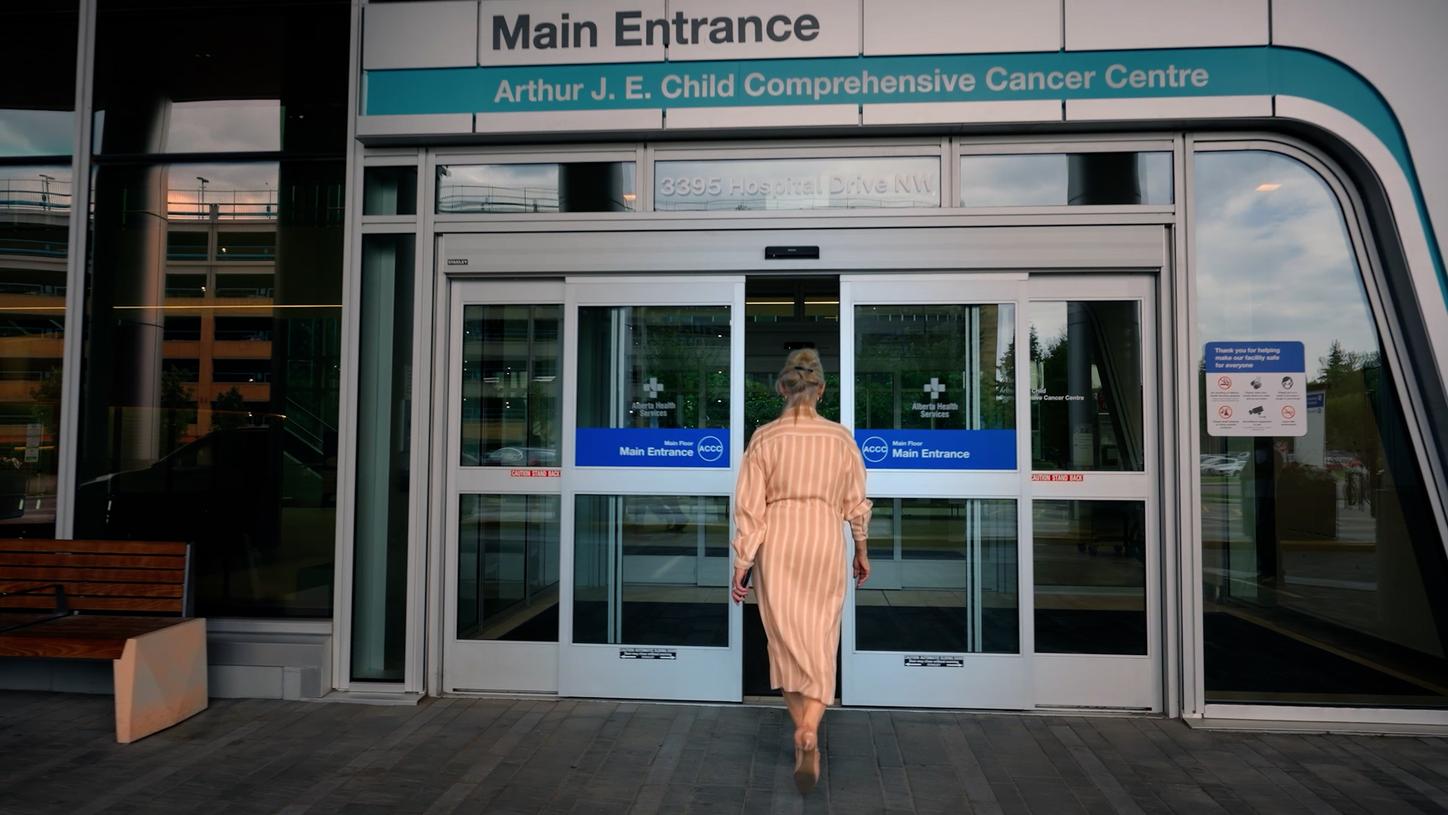
βÄ€This means ensuring patients have access to state-of-the-art care when they need it and that we tailor it to meet the needs of individual patients,βÄù says Brenda Hubley, chief program officer at Cancer Care Alberta.
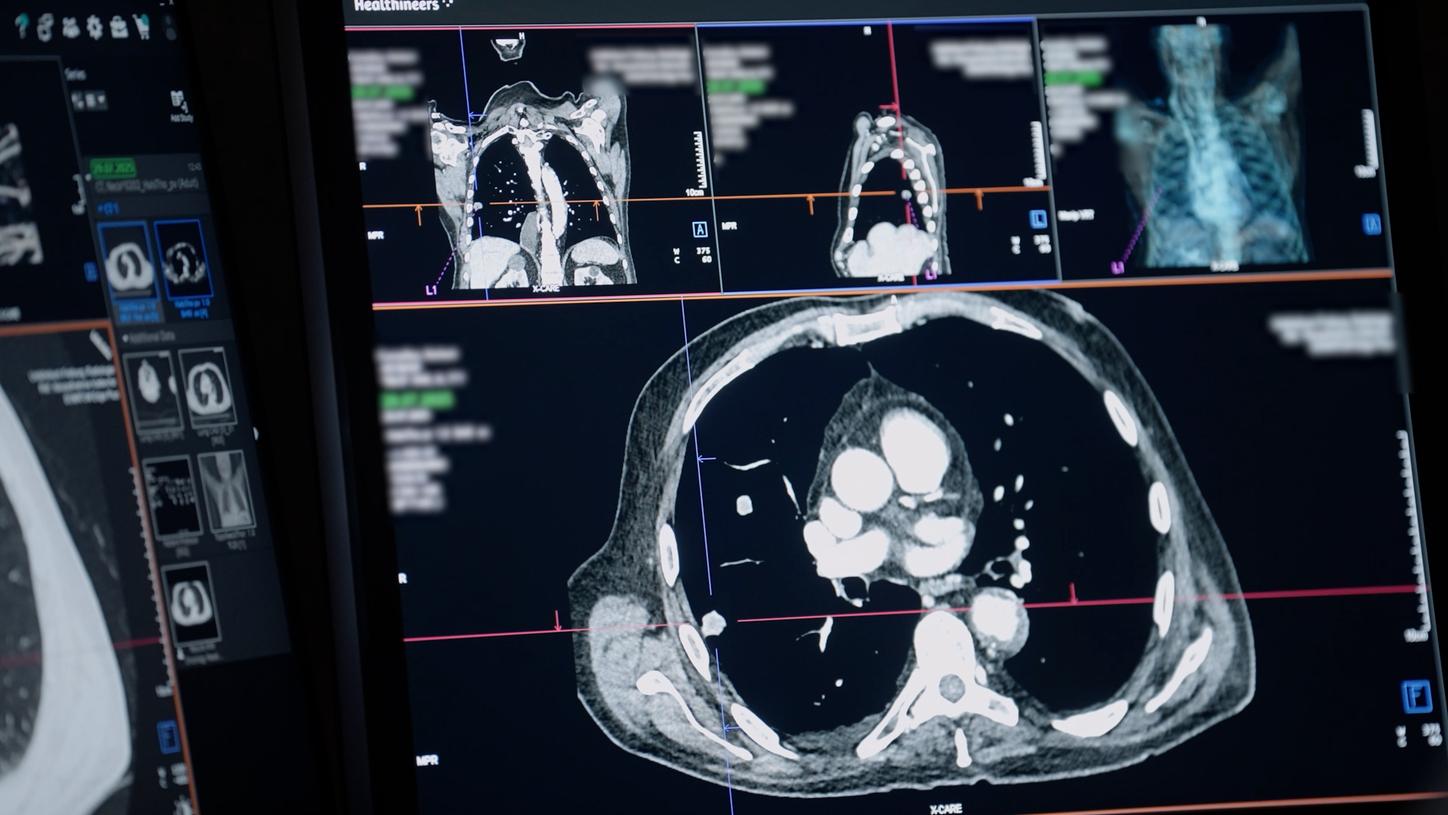
Beyond planning resources, AI is also transforming how clinicians understand disease itself. βÄ€Cancer is a nonlinear disease. With artificial intelligence, we can overcome the inherent limitations of linear models,βÄù says Omar Khan, MD, a medical oncologist at Cancer Care Alberta. The team has developed an AI model capable of extracting more than 5,000 features from CT images to predict survival outcomes in patients. βÄ€With our early data, the model is already a better predictor than staging,βÄù says Khan. βÄ€It goes beyond looking at cancer alone, but rather at the overall condition of the patient.βÄù
The true measure of progress isnβÄôt how intelligent systems become βÄî itβÄôs how much more human healthcare can be. βÄ€To me, the best way that care teams and health systems can support the cancer patient is recognizing that the cancer patient and their families are the experts on them,βÄù says Charlotte Kessler, patient and family advisor at Cancer Care Alberta, who was diagnosed with a rare form of brain cancer in 2013. βÄ€We know how we are feeling, we know what we are experiencing when we are listened to, heard, and engaged. We feel empowered, and by feeling empowered, we are able to face cancer from a much stronger stance.βÄù