Tackling stroke with speed and precision
Facts




Diagnosis
Recognizing early warning signs โ FAST
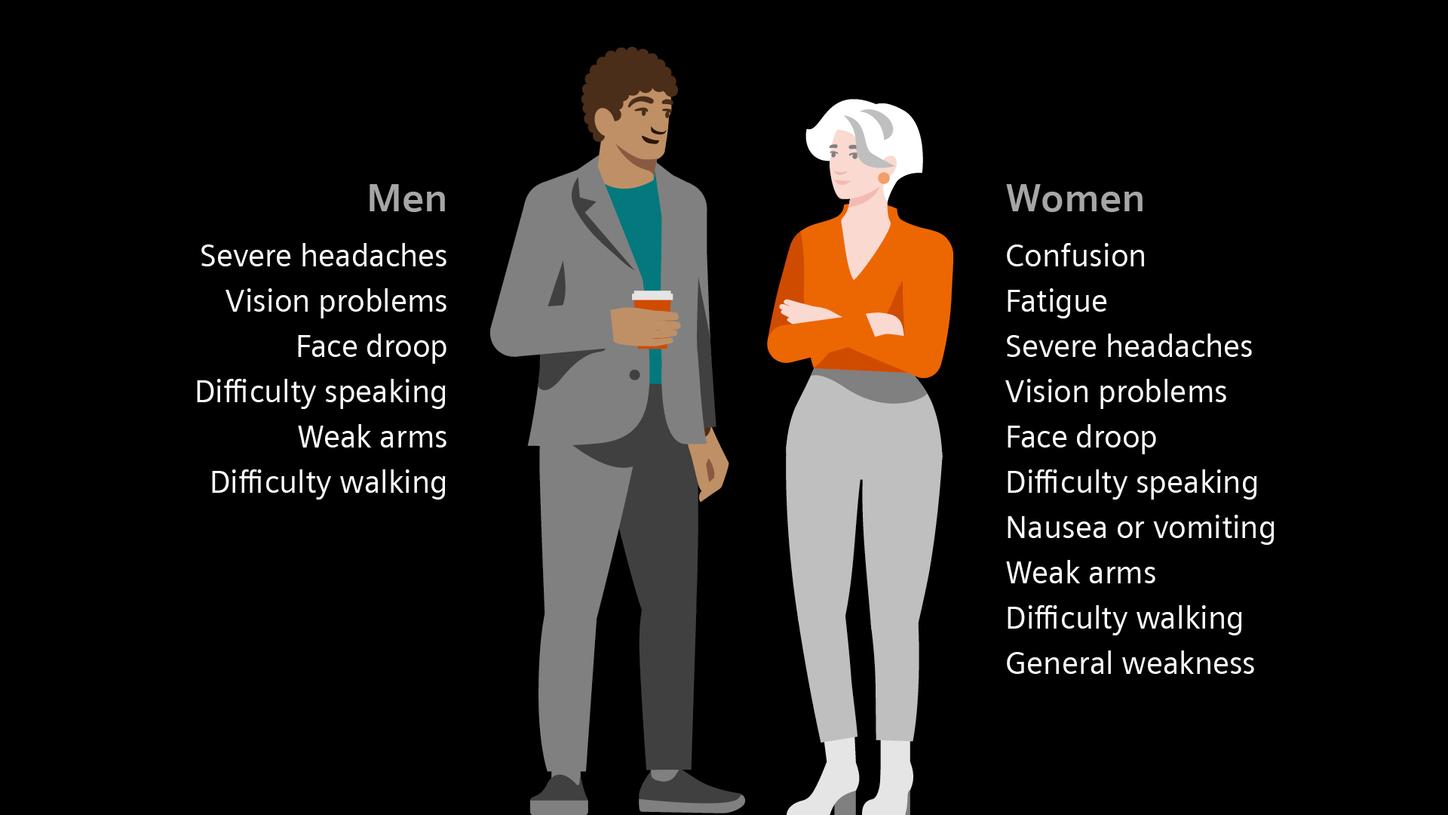
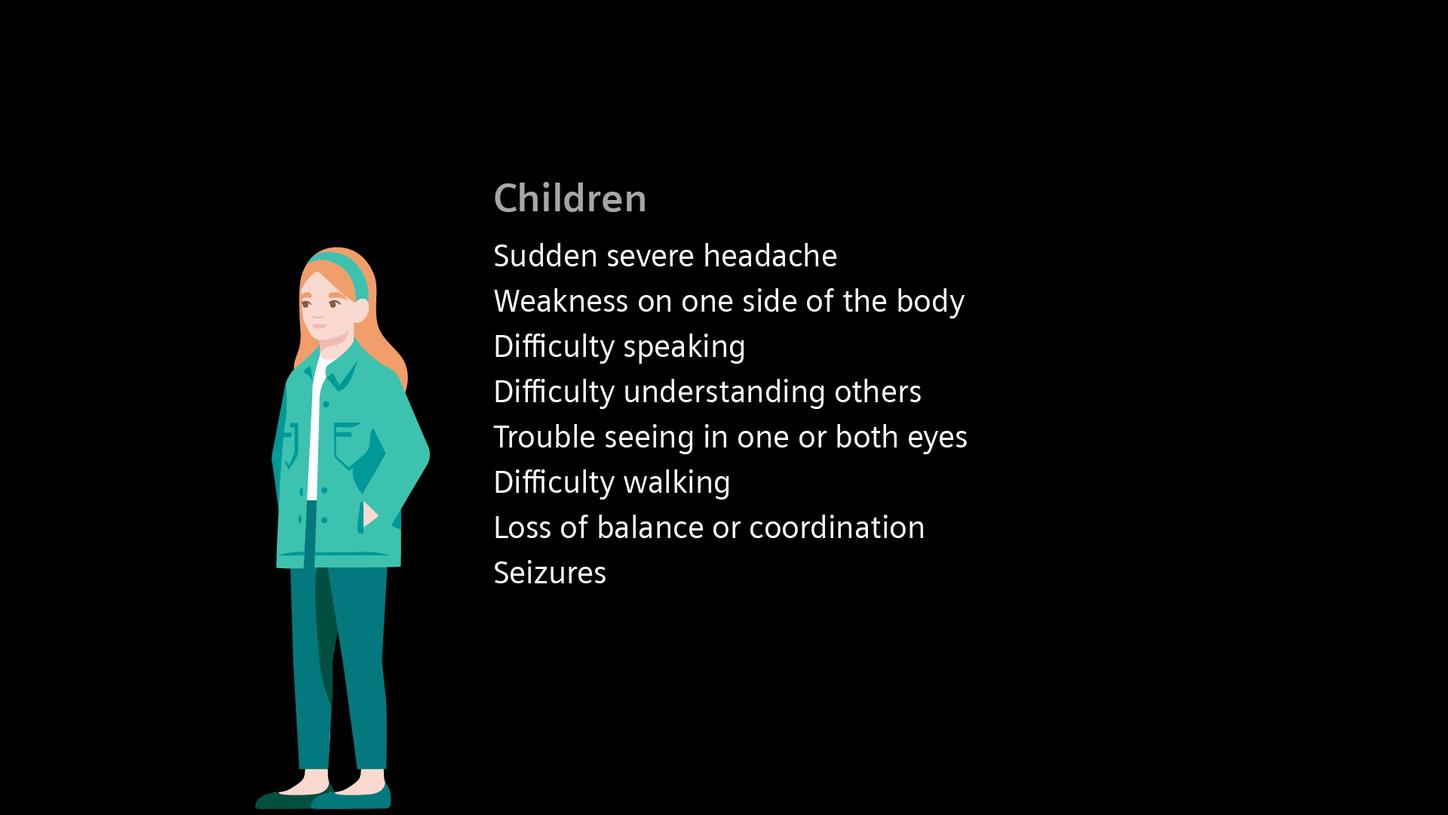
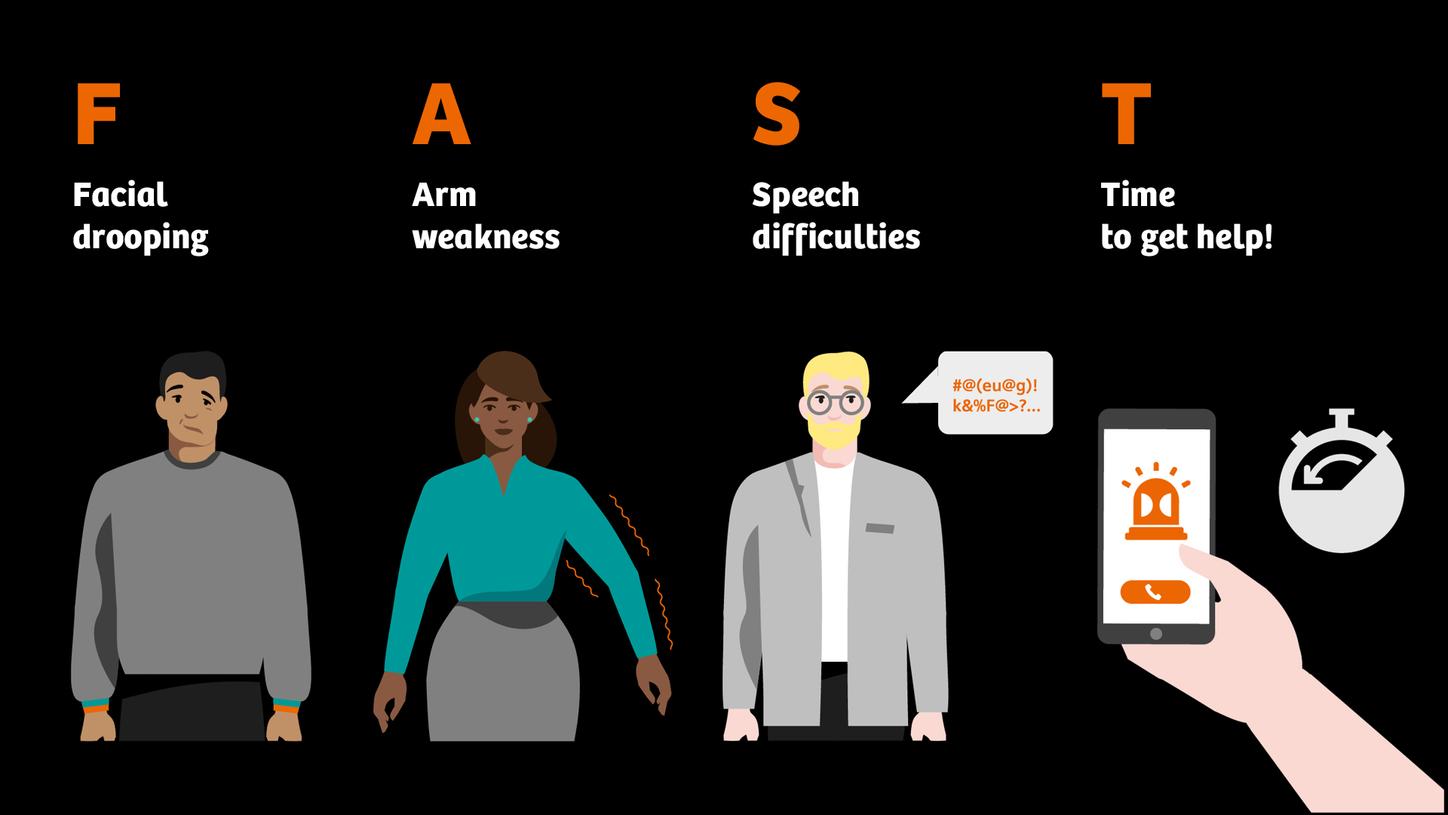
The sooner treatment begins after the onset of stroke symptoms, the better the chance of preventing permanent damage. Recognizing early warning signs โ like sudden weakness or numbness on one side, slurred speech, or vision disturbances โ can be life-saving. The easy to remember FAST test (Face, Arms, Speech, Time) provides a quick and effective way to identify a potential stroke and act immediately.



Follow Mike on his acute stroke health journey
Stroke is a medical emergency where every second matters. Rapid and precise diagnosis is critical for effective treatment and improved outcomes. Mikeโs case (exemplary patient) illustrates what optimal stroke care can look like.
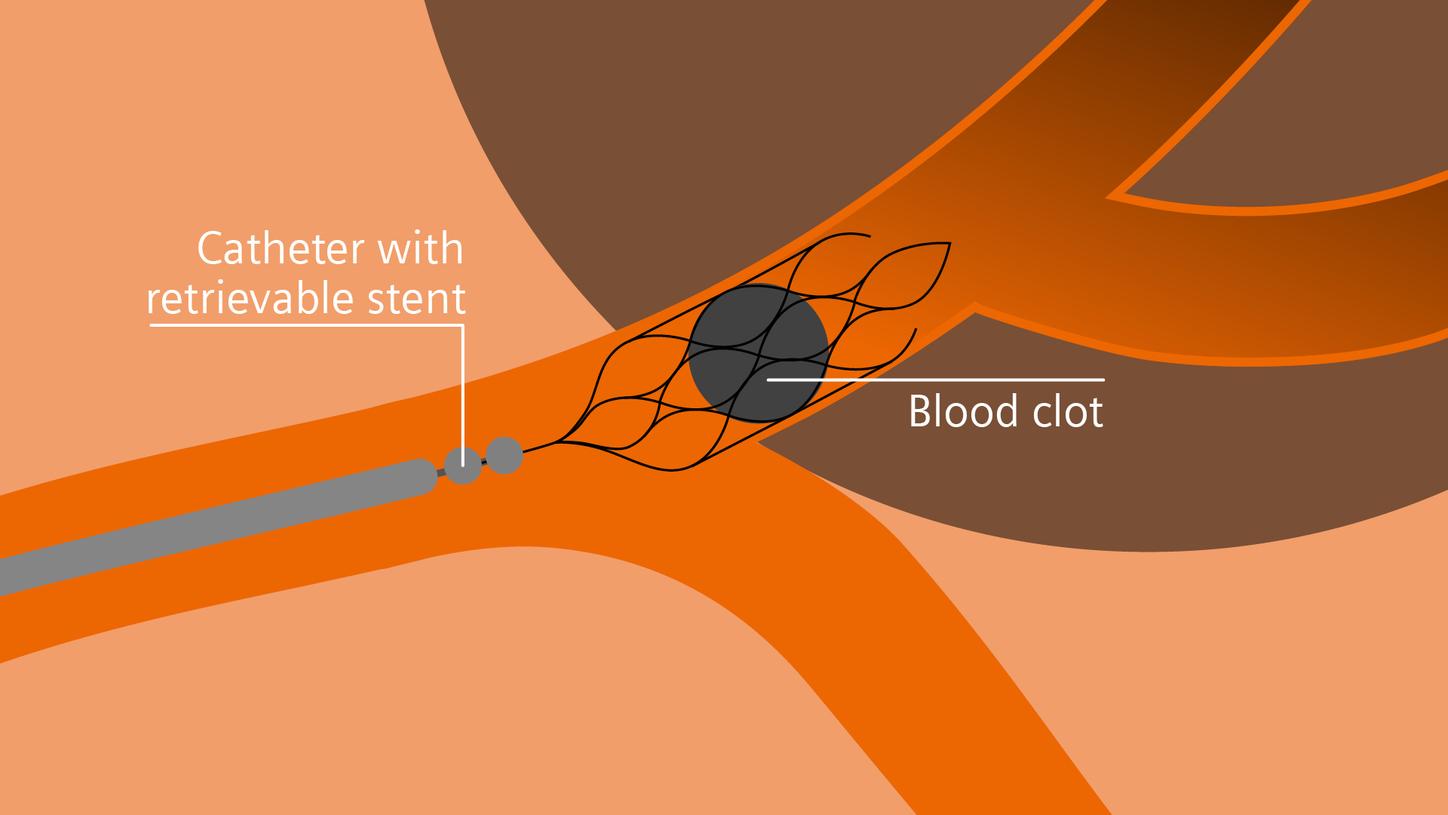
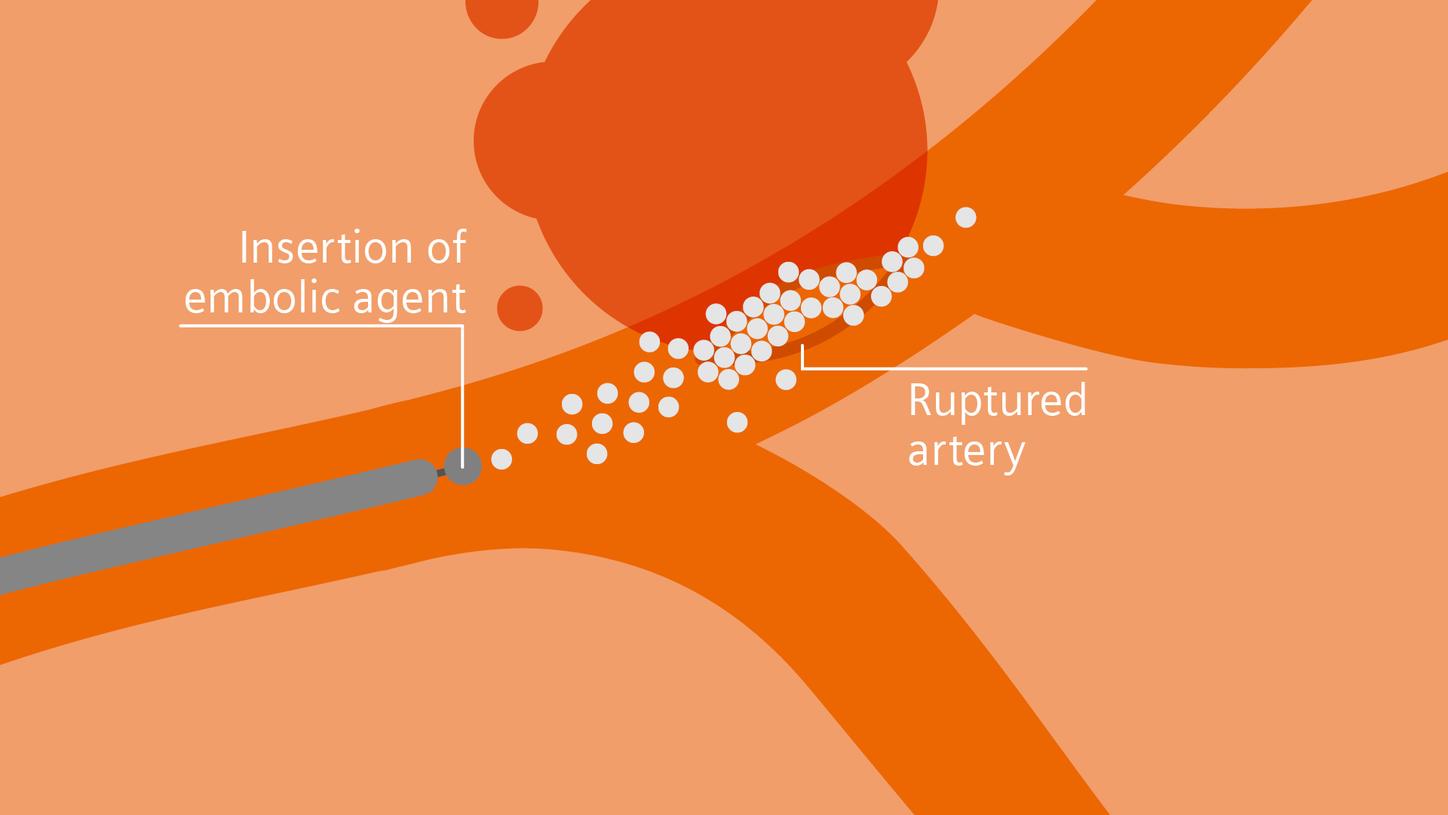
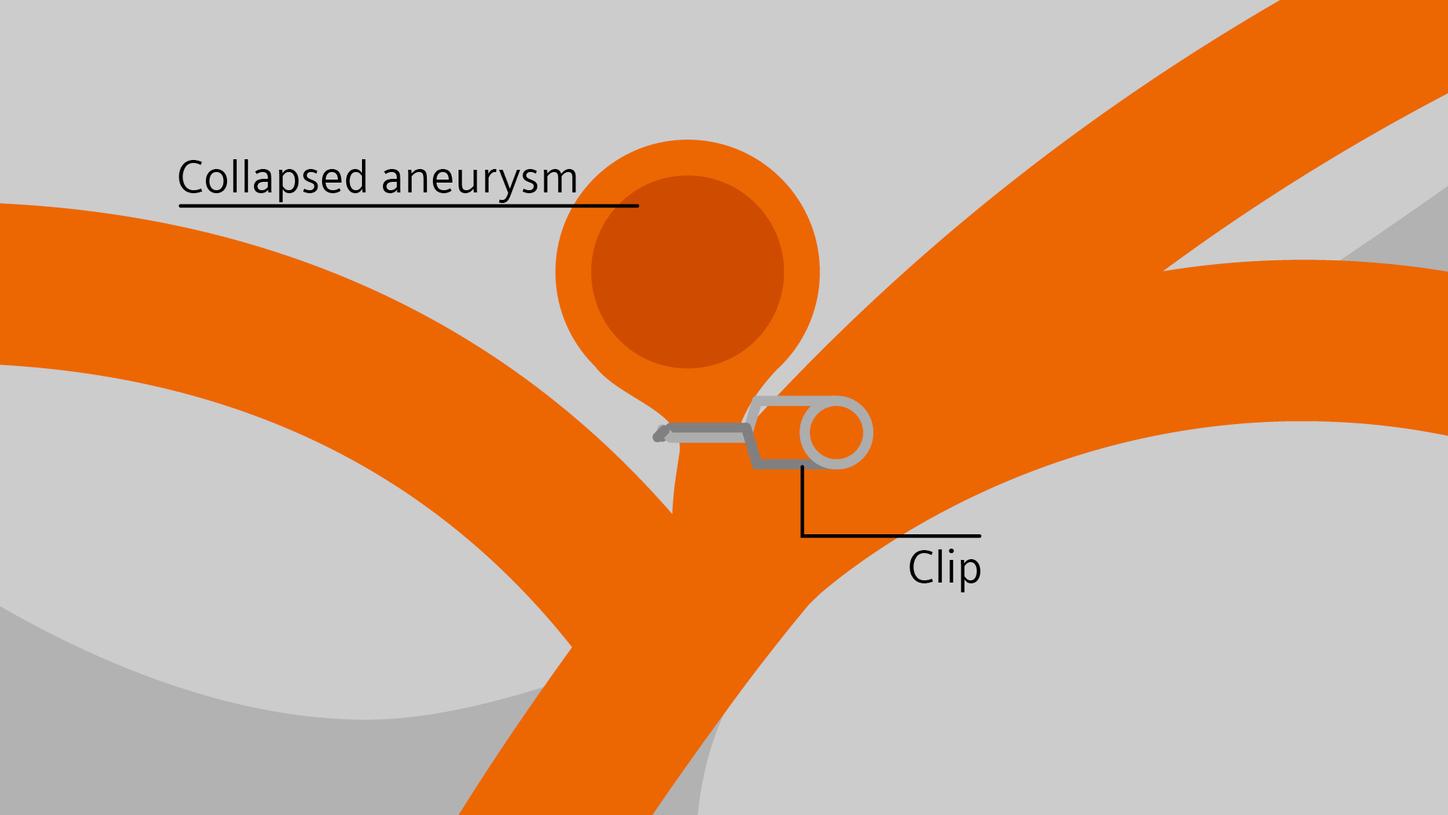
Treatment
Critical insights in seconds:
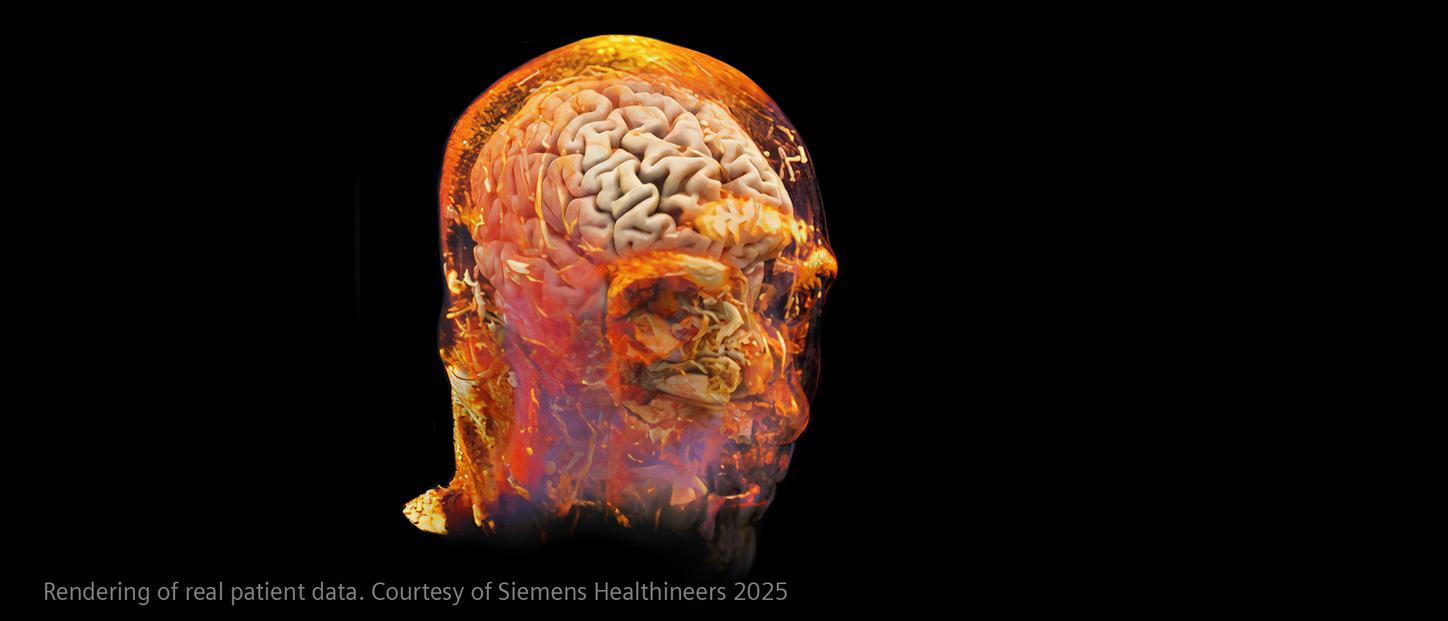
How advanced imaging and AI transform stroke workflow
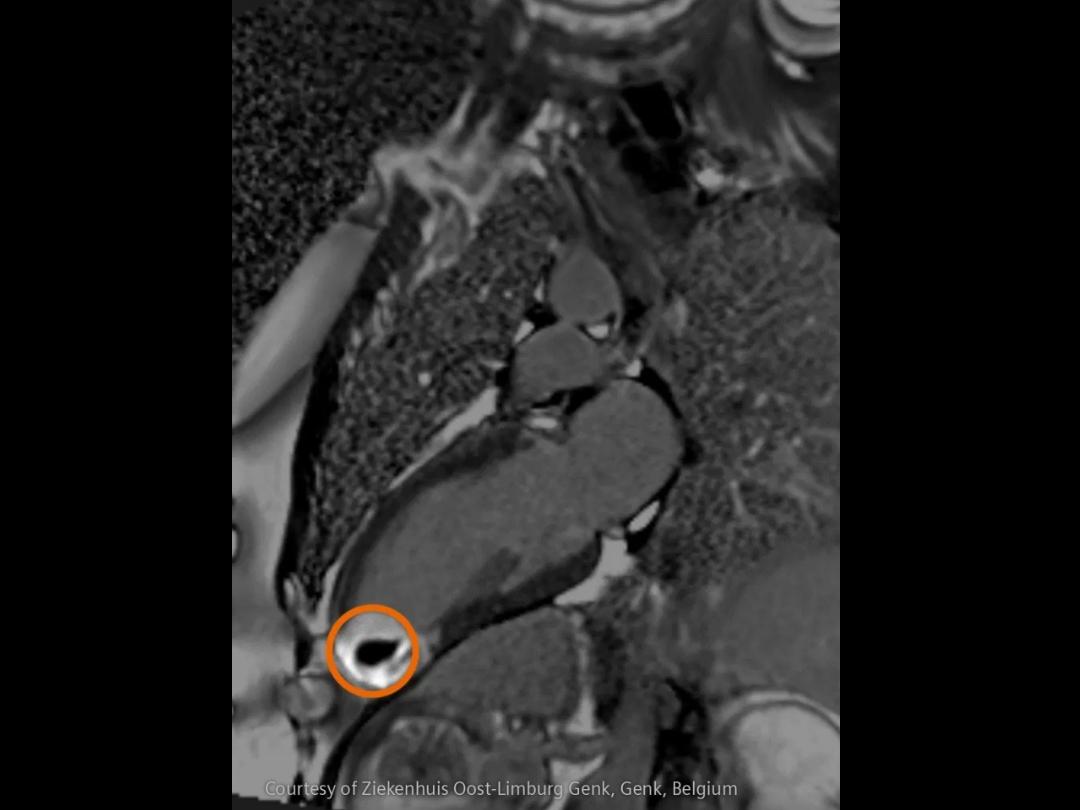
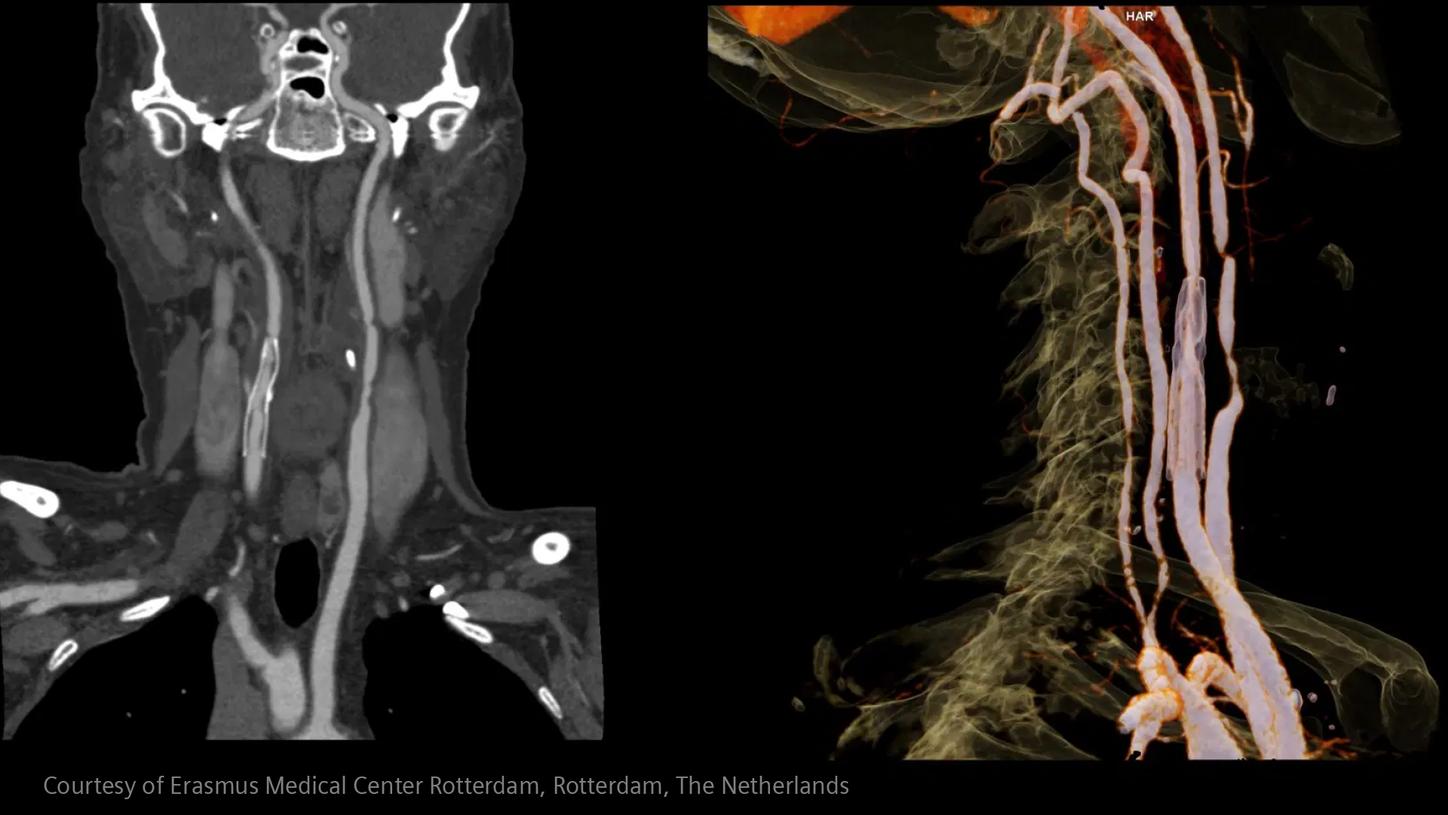
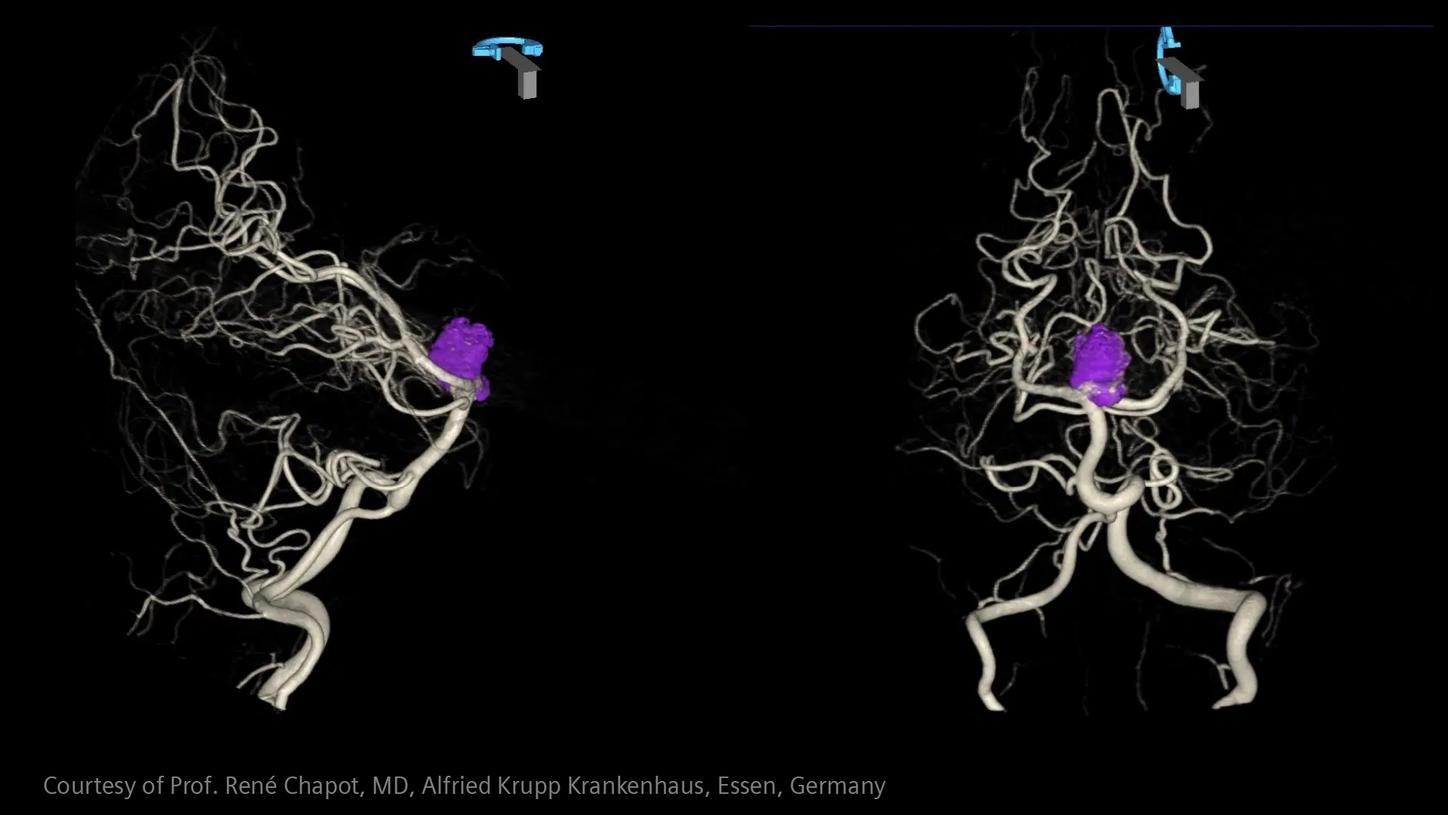
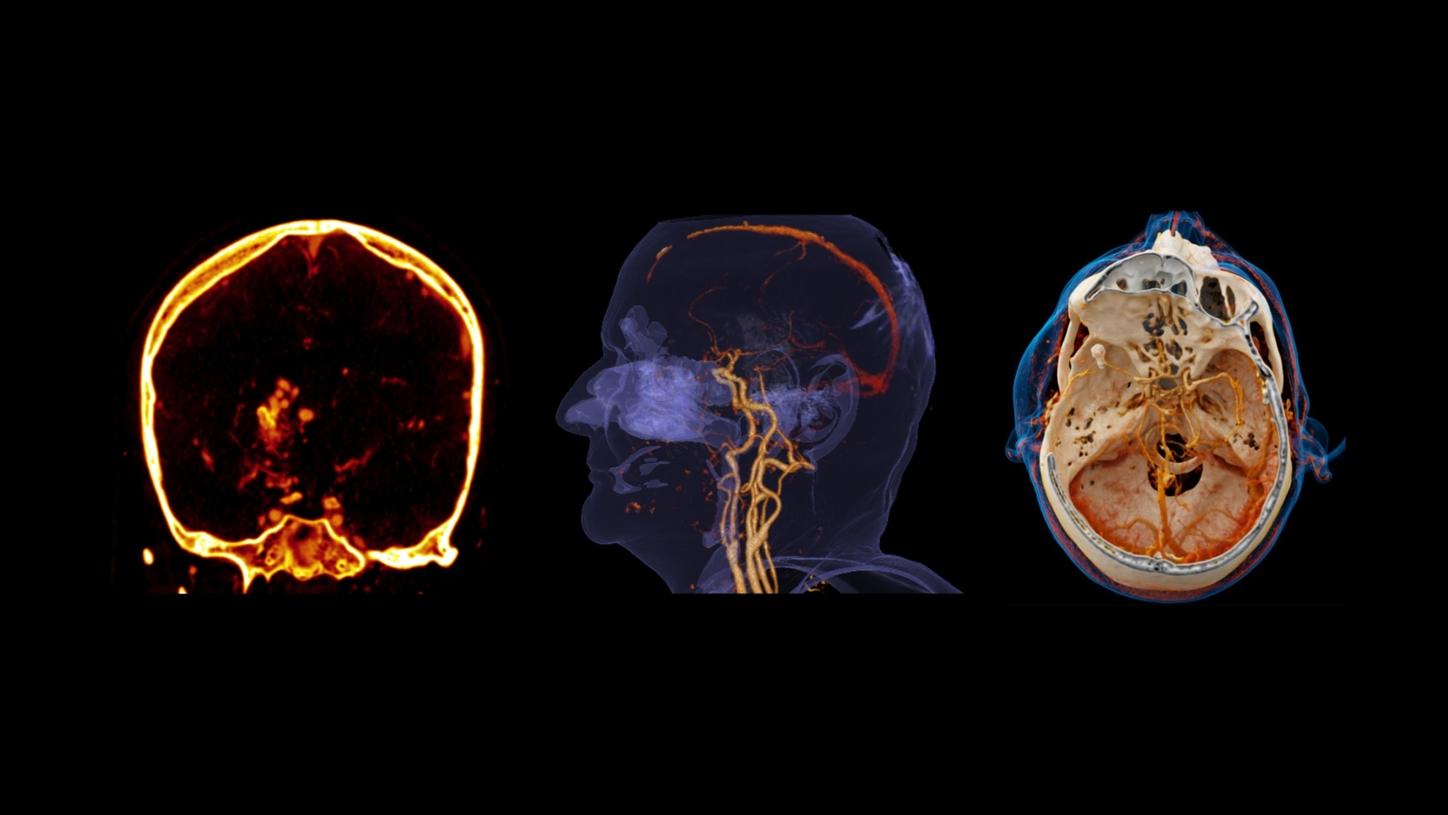
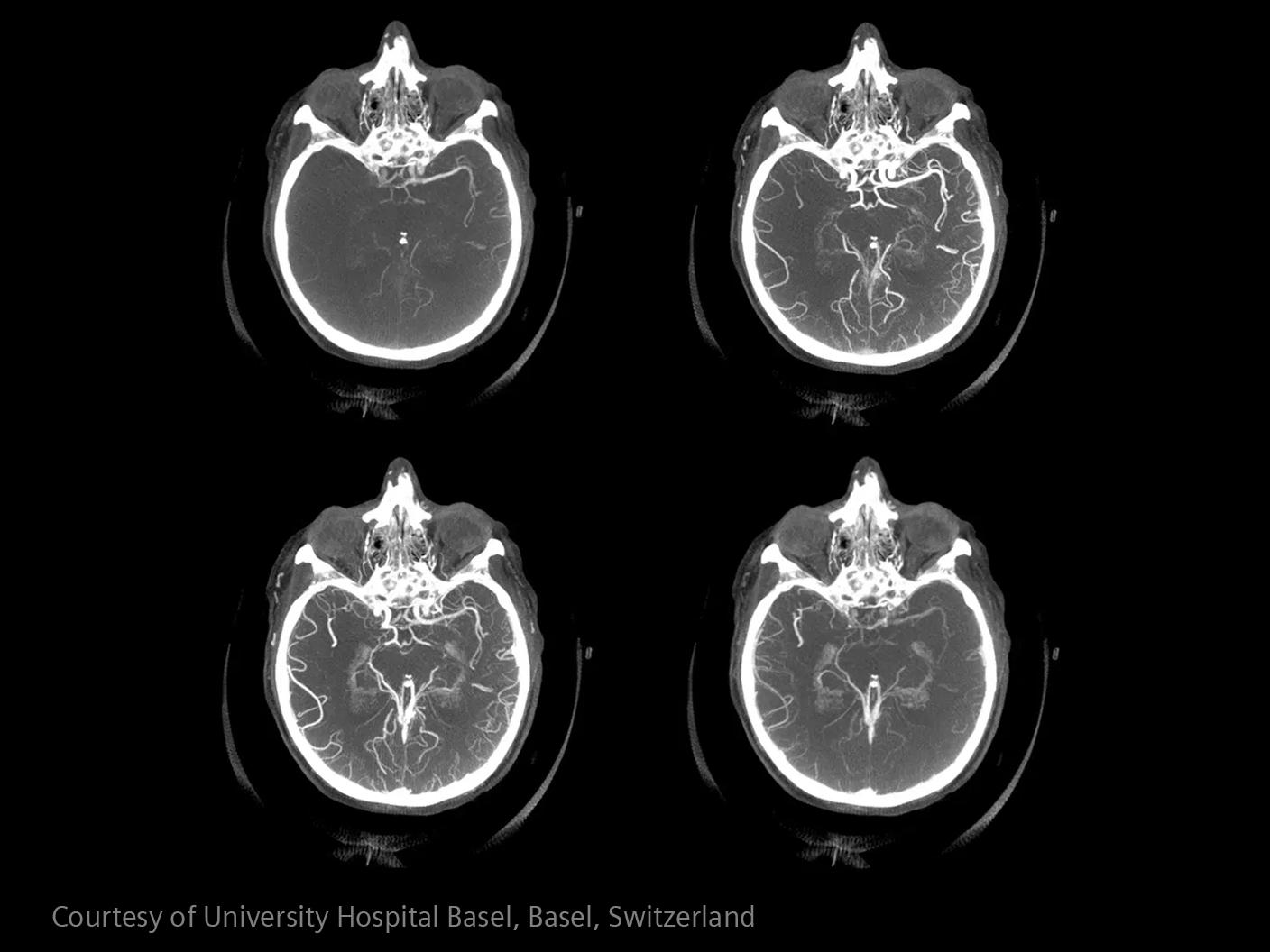
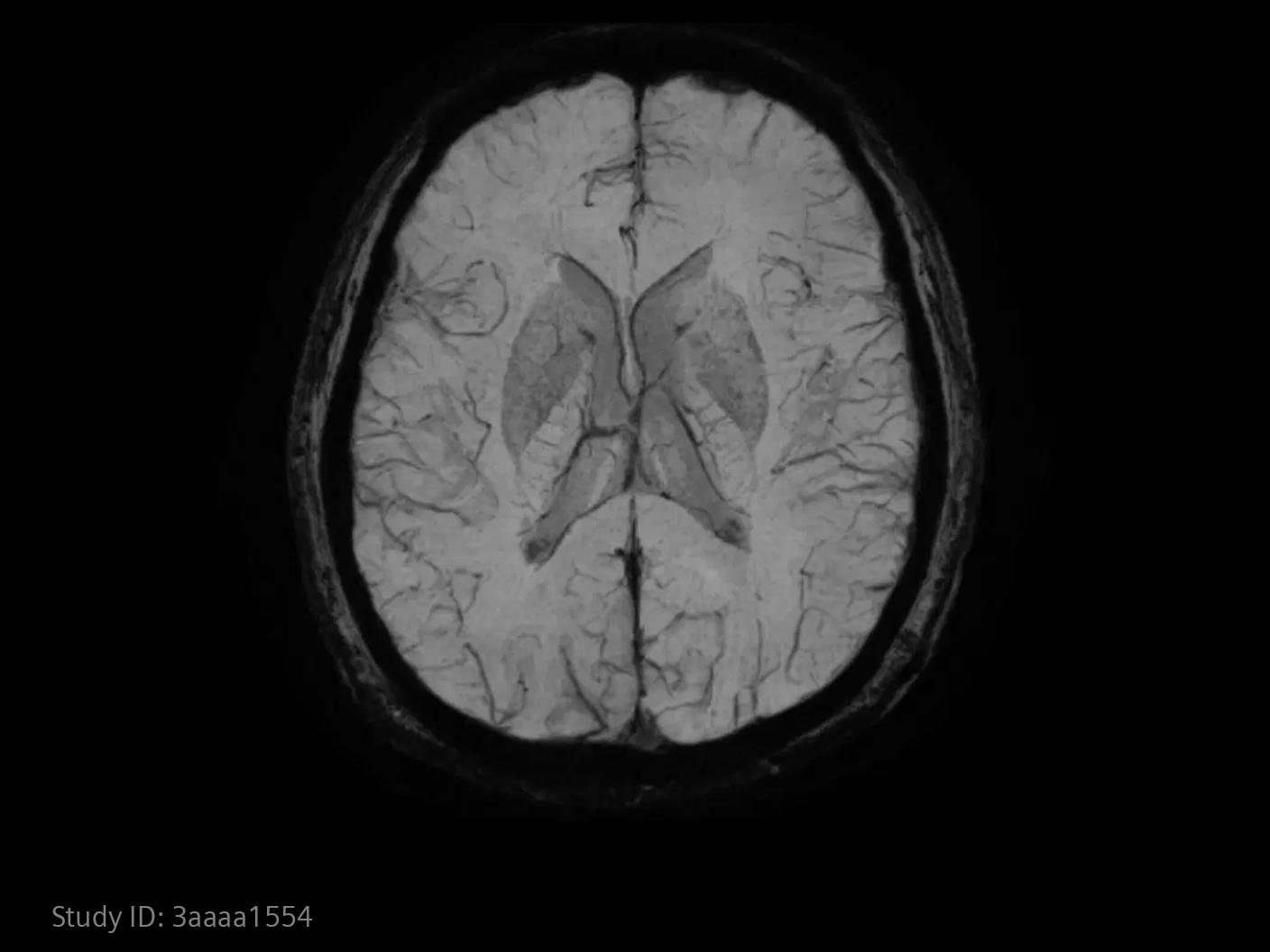
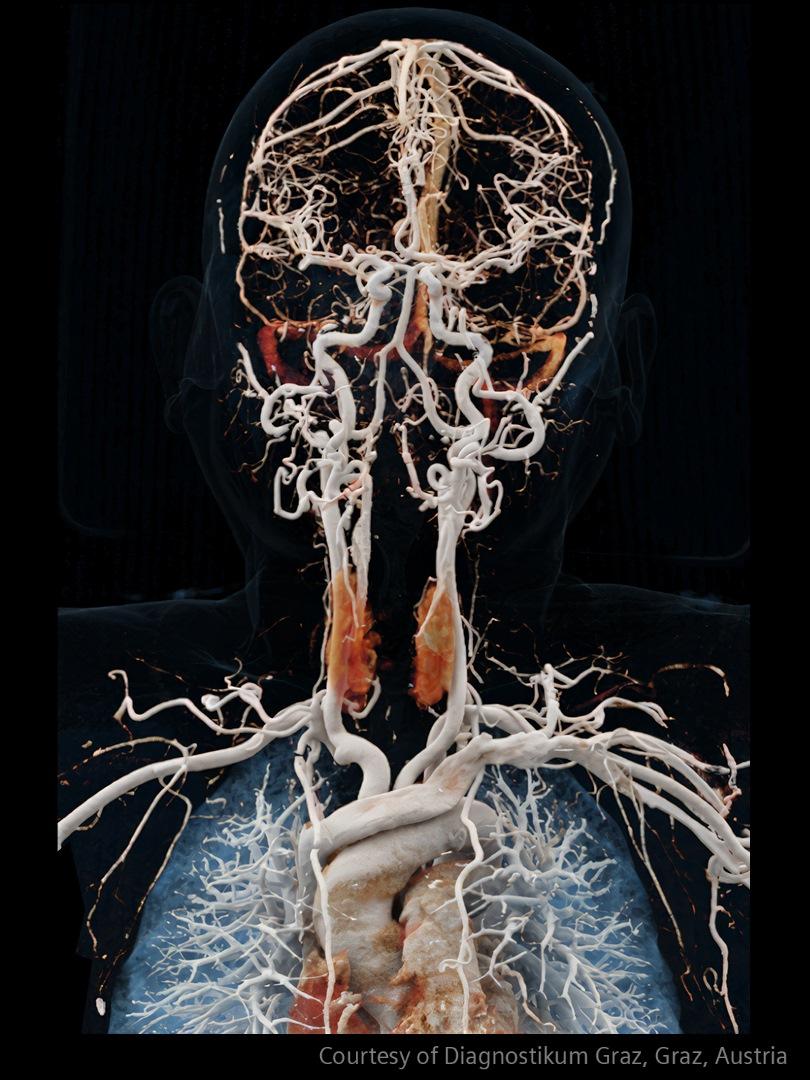
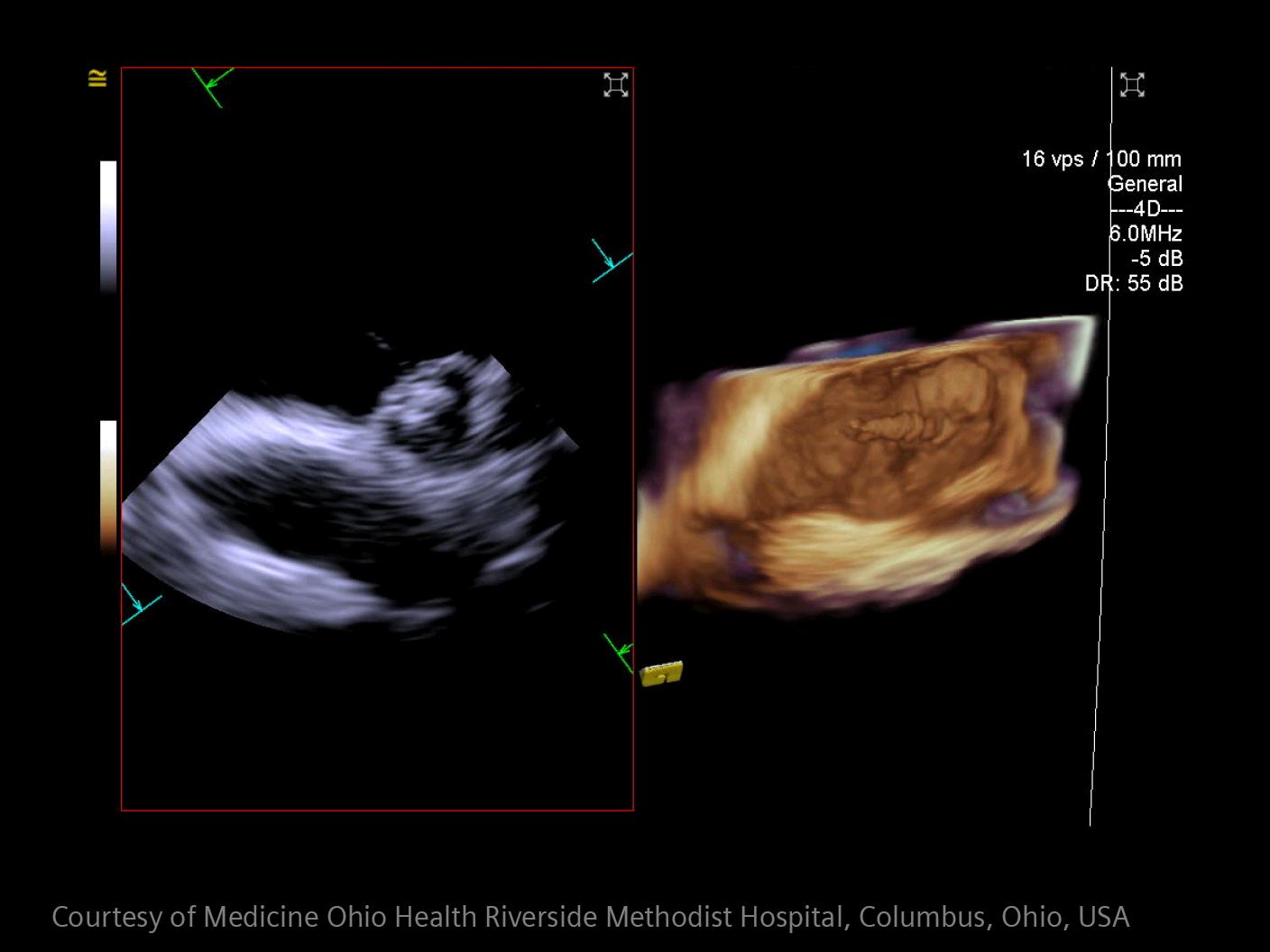
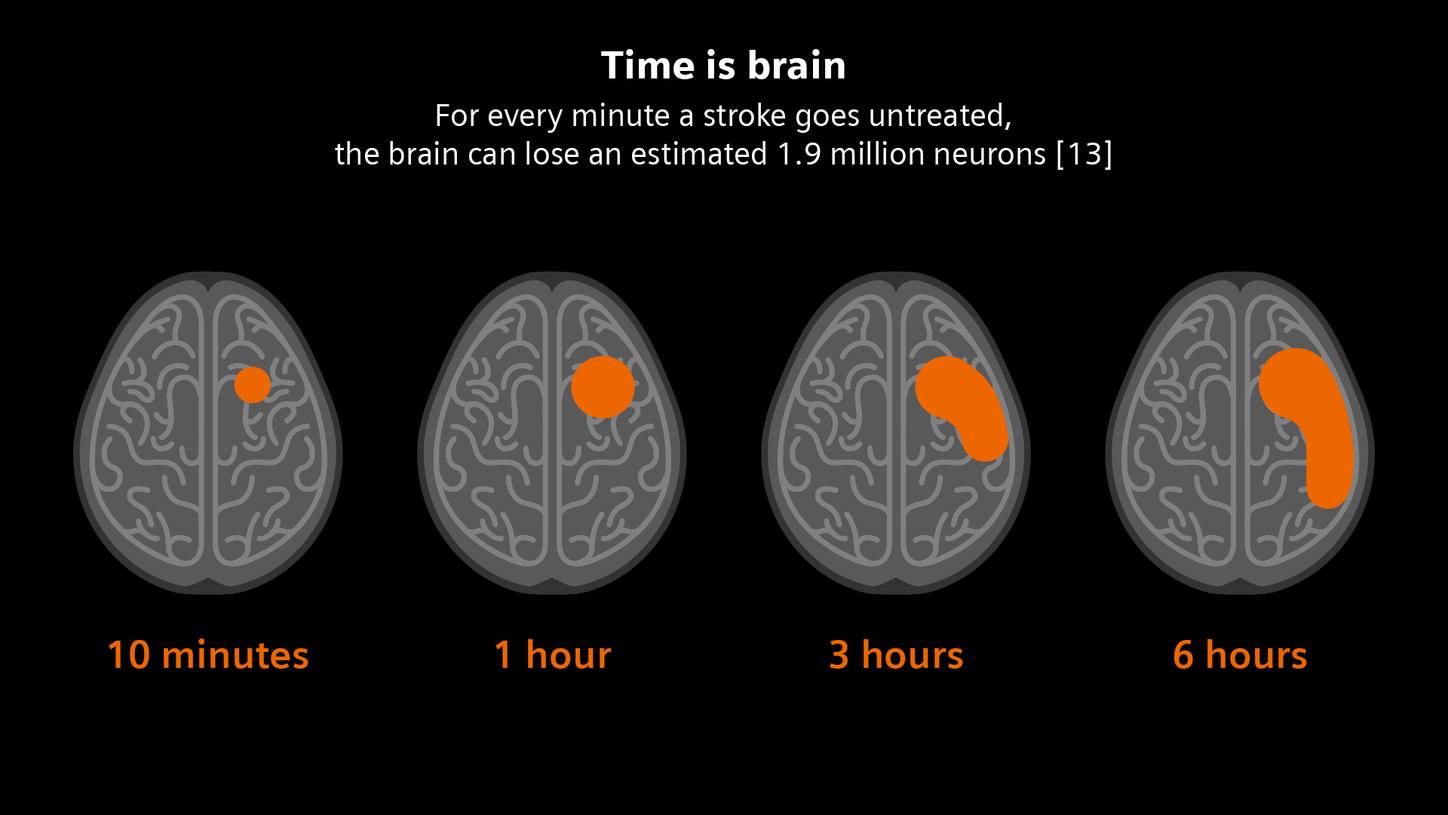
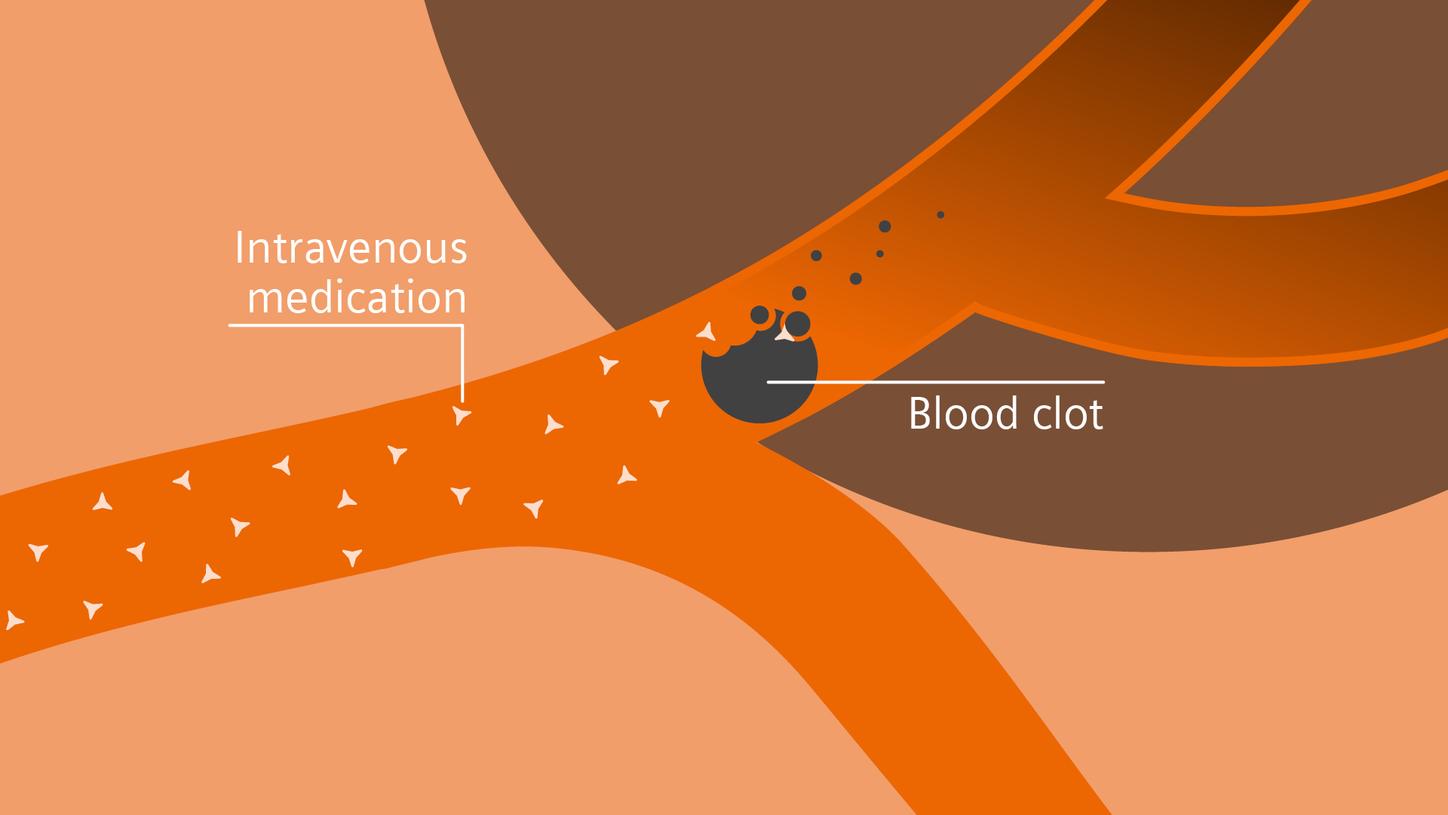
In stroke care, time is brain. Rapid and accurate imaging is crucial to assess the extent of brain injury and guide immediate treatment. Angiography, MRI, CT, ultrasound, and lab diagnostics are essential tools in identifying stroke type, location, and severity. Advances in imaging technology now allow for even faster acquisition, improved resolution, and enhanced visualization of brain tissue and blood vessels. Innovations such as perfusion imaging, real-time vascular mapping, and AI-assisted diagnostics are transforming stroke workflows and enabling precise, timely interventions.


Aftercare
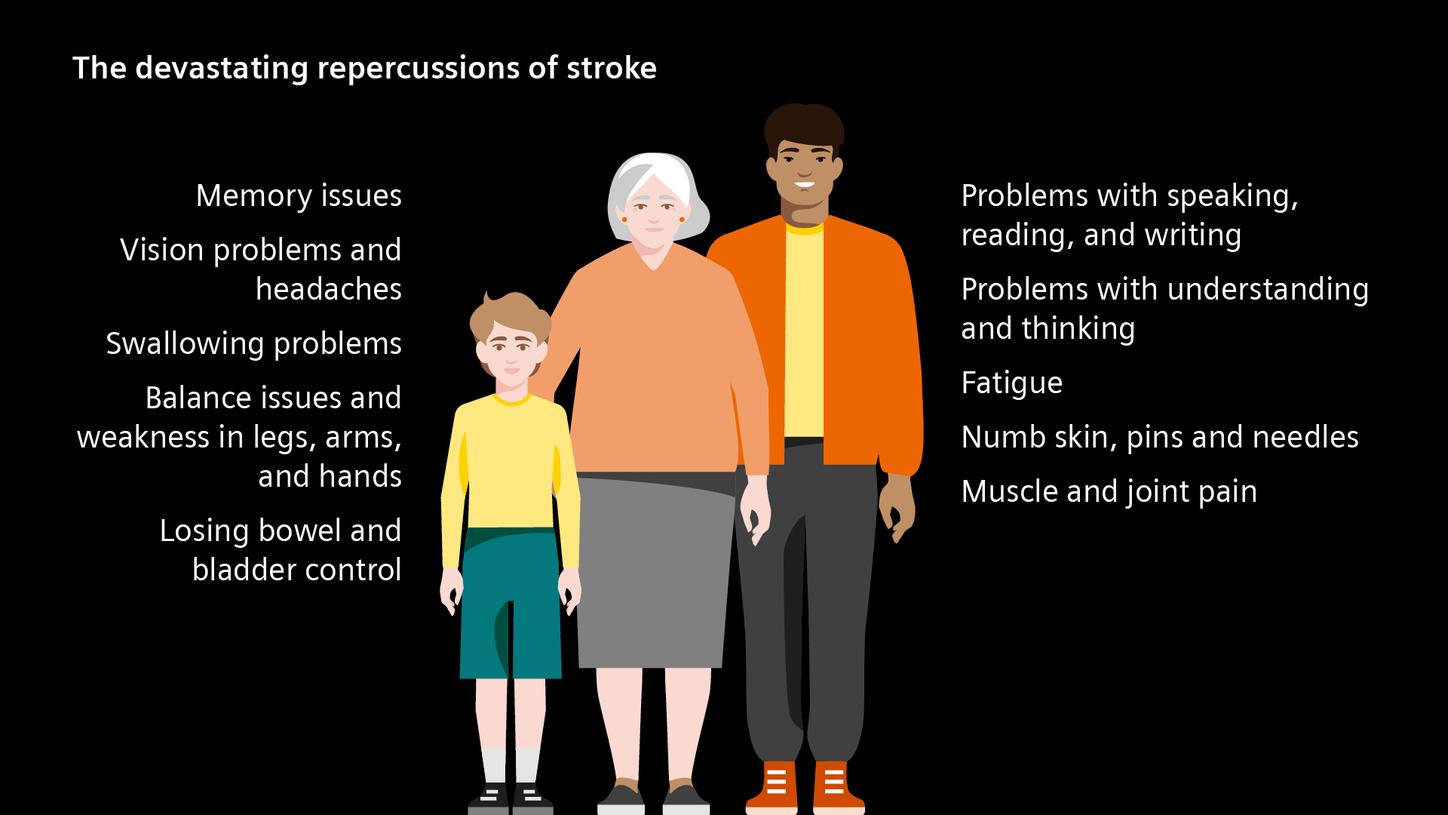
Strong again โ long-term care and secondary stroke prevention
[1] Feigin VL, Brainin M, Norrving B, Martins SO, Pandian J, Lindsay P, et al. World Stroke Organization: Global Stroke Fact Sheet 2025. Int J Stroke [Internet]. 2025;20(2):132โ44. Available from:
[2] Rรผcker V, Heuschmann PU, OโFlaherty M, Weingรคrtner M, Hess M, Sedlak C, et al. Twenty-year time trends in long-term case-fatality and recurrence rates after ischemic stroke stratified by etiology. Stroke [Internet]. 2020;51(9):2778โ85. Available from:
[3] Impact of stroke [Internet]. World Stroke Organization. [cited 2025 Jun 5]. Available from:
[4] CDC. Stroke facts [Internet]. Stroke. 2024 [cited 2025 Jun 11]. Available from:
[5] dsg_adm. Europรคischer Aktionsplan ausgerufen [Internet]. Deutsche Schlaganfall-Gesellschaft. 2022 [cited 2025 Jun 11]. Available from:
[6] GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol [Internet]. 2021;20(10):795โ820. Available from:
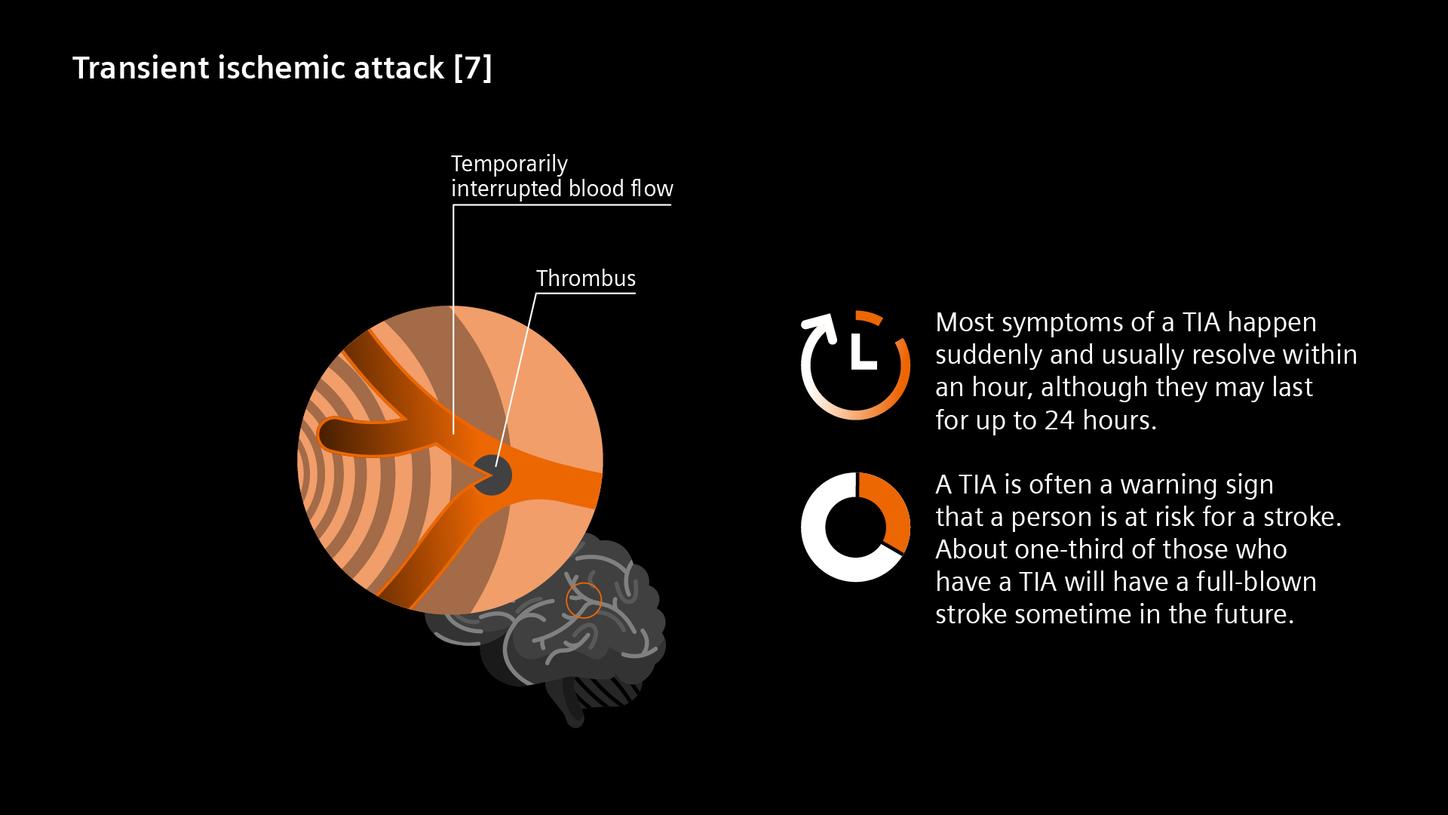
[7] Transient ischemic attack (TIA) [Internet]. National Institute of Neurological Disorders and Stroke. [cited 2025 Jun 12]. Available from:
[8] Elisabeth P. What women need to know about stroke [Internet]. Mayo Clinic Press. 2024 [cited 2025 Jun 5]. Available from:
[9] British Heart Foundation. High blood pressure during pregnancy increases risk of heart attacks and strokes [Internet]. British Heart Foundation. 2019 [cited 2025 Jun 5]. Available from:
[10] Oral contraceptives and hormone therapy increase the risk of stroke [Internet]. Www.uu.se. [cited 2025 Jun 5]. Available from:
[11] deVeber GA, Kirton A, Booth FA, Yager JY, Wirrell EC, Wood E, et al. Epidemiology and outcomes of arterial ischemic stroke in children: The Canadian Pediatric Ischemic Stroke Registry. Pediatr Neurol [Internet]. 2017;69:58โ70. Available from:
[12] Stroke.org. [cited 2025 Jun 5]. Available from:
[13] Saver JL. Time is brain--quantified. Stroke [Internet]. 2006;37(1):263โ6. Available from:
[14] Deutscher รrzteverlag GmbH. The frequency and timing of recurrent stroke [Internet]. Deutsches รrzteblatt. [cited 2025 Jun 5]. Available from:
[15] Arsava EM, Helenius J, Avery R, Sorgun MH, Kim G-M, Pontes-Neto OM, et al. Assessment of the predictive validity of etiologic stroke classification. JAMA Neurol [Internet]. 2017;74(4):419โ26. Available from:
[16] Research, Markets ltd. Brain Aneurysm Treatment Market Forecast to 2027 - COVID-19 Impact and Global Analysis by Type; Condition; End User, and geography [Internet]. Researchandmarkets.com. [cited 2025 Jun 18]. Available from:
[17] Stroke.org. [cited 2025 Jun 5]. Available from:
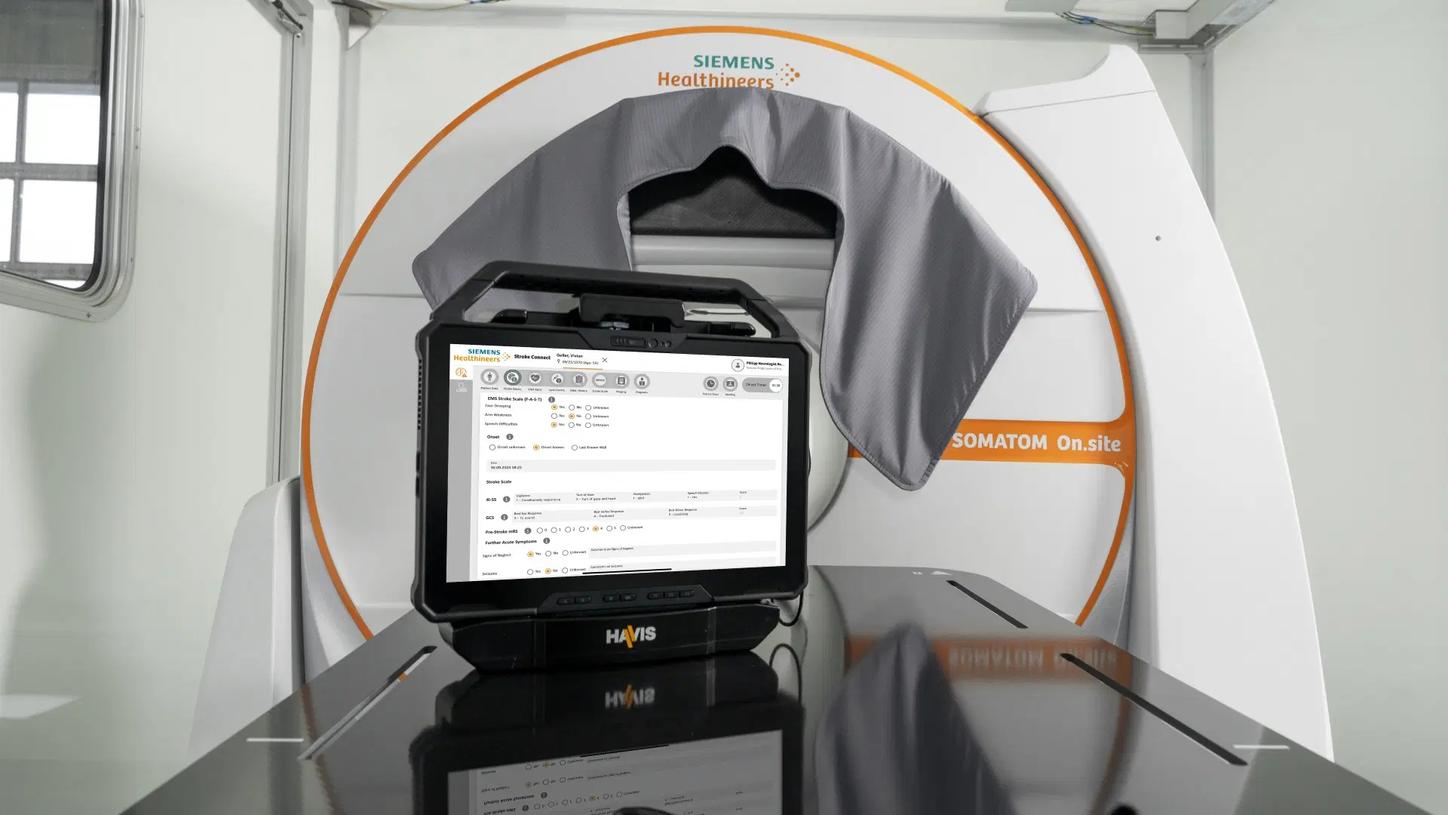
1 SOMATOM On.site is not commercially available in all countries. Its future availability cannot be guaranteed.
2 Stroke Connect contains medical and non-medical devices. This solution cannot be used directly for diagnostic purposes. Product availability may vary from country to country and is subject to varying regulatory requirements. Please contact your local representative for availability. Stroke Connect is not currently available in the US. Adaptation for US requirements is in progress, with no guaranteed availability.
3 Not commercially available in the US.
The products/features mentioned herein are not commercially available in all countries. Future availability cannot be guaranteed.